Eco-ALS and mechanical chest compressions: that’s the way I like to run a code
47 ysr old male collapsed on the field. First ALS unit found him arrested in VF.
Shocked 3 times he regained a palpable central pulse.
When we arrived the patient arrested again. VF on the monitor. Shocked 4 times. Mechanical chest compression and tracheal intubation on board. He received Epi, Amio (300+150), Calcium Gluconate and Bicarb (suspected iper K in kidney insufficiency) before the ROSC.
15 minutes passed from the collapse to ROSC, 7 of wich were of “no flow” (no chest compressions, no AED from bystanders).
PMH: Hypertension, kidney insufficiency, heavy smokers. Medication history unknown.
He had chest pain before collapsing, as referred from bystanders.
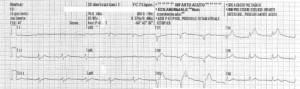
Vitals at ROSC: GCS 3 T, RR 10 MV, SaO2 100%, EtCO2 35, HR 70 bpm. NIBP 100/70 12 lead EKG at ROSC is shown below.
An echo of the heart performed on the field (in the ambulance running to the ED, so I apologize for the low quality of the images) confirmed the lateral wall MI and shown distended IVC, B lines in both lungs and no sign of aortic dissection. No free fluid was present in the abdomen.
After administration of Heparin and Aspirin the patient arrived in ED and taken straight to cat-lab where a PTCA was performed 50 min after the collapse.
I think that increasing the use of ultrasonography on the field, and using it when really makes the difference, with a Point Of Care approach, is a big step for the care of critical patients out of the hospital.
Every prehospital emergency system have to instruct their professionals on how to use POC Ultra Sonography on the field and need specific “problem solving” protocols to help it’s diffusion.