Tachycardia: important things to keep in mind for treatment
Tachycardia simply means a faster heart rate than normal. With the sinoatrial node, which is the heart’s inborn pacemaker, the intrinsic rate is between 60 and 100 beats per minute. When the rate exceeds 100 beats per minute, tachycardia is present.
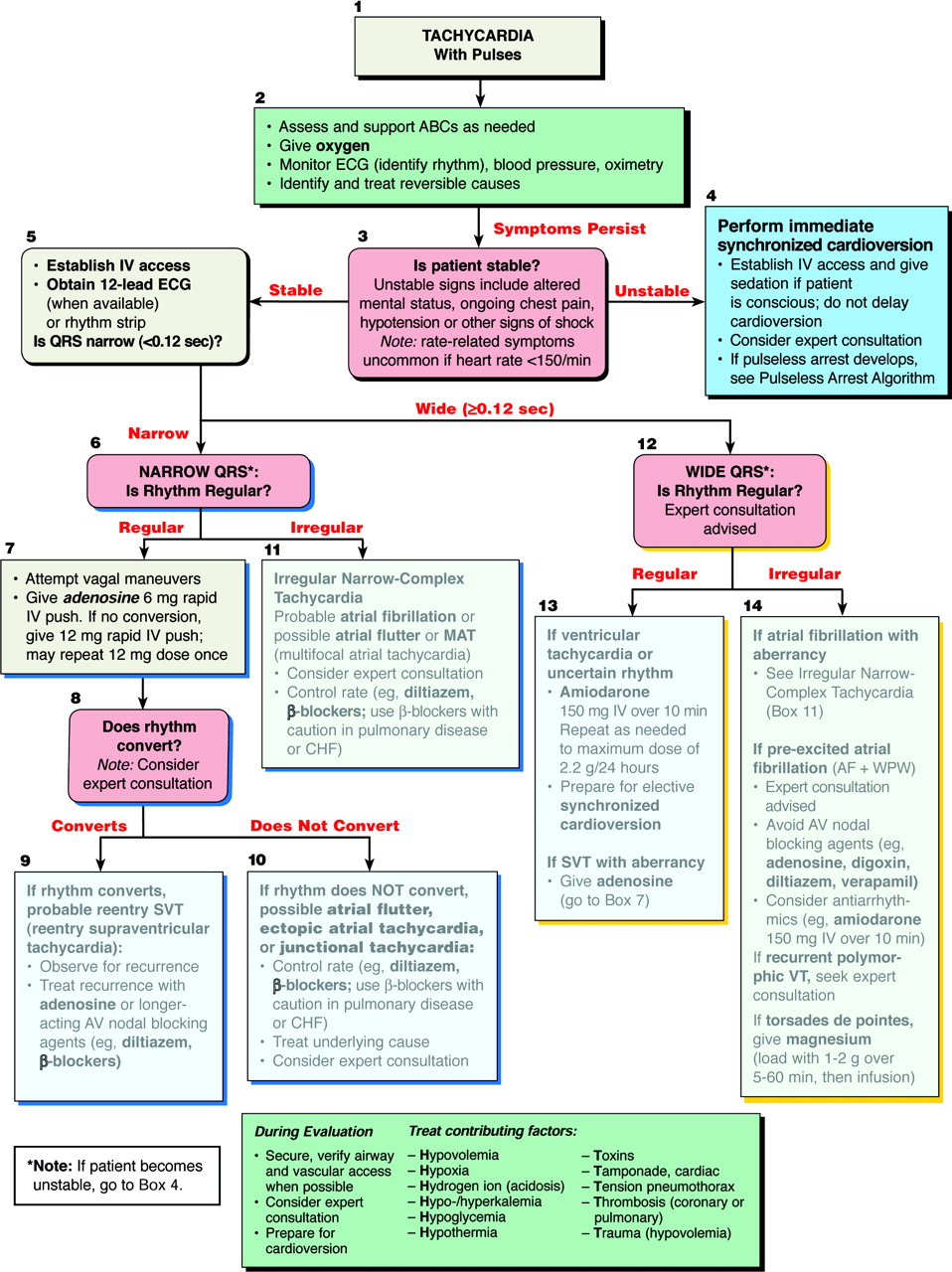
When treating tachycardia, it is important to first consider a compensatory cause. The body tends to use an increased heart rate as a frequent compensatory mechanism when it senses decreased perfusion.
Two of the best dysrhythmics in the EMT and paramedic’s tool box are OXYGEN and NORMAL SALINE. Both of these treatments should be attempted prior to using any other medication. It is not advantageous to eliminate a compensatory tachycardia in a patient who needs it to perfuse. Locating the cause of the decreased perfusion would be optimal.
Another thing to consider is the patient’s hemodynamic stability. With organized tachycardic rhythms in unstable patients, synchronized cardioversion is indicated. There seems to be a fear amongst prehospital providers when it comes to shocking people.
The paramedic seems to be much more comfortable giving anti-arhythmic/dysrhythmic medications than they do performing cardioversion. This is in-fact backwards thinking. Consider Kelly Grayson’s outlook on dysrhythmic drugs – they are selective cardiotoxins. First off, they are not naturally found in the body. Second, they metabolize over time and the reaction can be unpredictable. Thirdly, they are used to counteract cellular depolarization.
Do you know what happens in the absence of cellular depolarization in the myocardium? Asystole – not a common side effect, but it drives home the point doesn’t it? Other complications, like high-grade atrioventricular blocks, and long QT syndrome may also occur.
Conversely, synchronized cardioversion doesn’t have nearly as many unwanted effects. It works fast, and goes away. The medication you should be considering, is some sort of sedative or benzodiazapine prior to cardioversion.
Next, after determining the patient’s hemodynamic stability, the width of the QRS should be considered. If the patient is stable, and they are in a sustained tachycardia, dysrhythmic medications can be considered.
It is important to determine the width of the QRS, because medications like Cardizem (diltiazem), or Adenocard (adenosine) that may be administered to narrow complex rhythms, can effectively KILL people with wide QRS rhythms.
Notice that there is not a ‘ventricular tachycardia’ algorithm? It states ‘Wide QRS’, and lists ‘uncertain rhythm’ below. This is an important concept. If it is wide, and you are uncertain of the origin, it is ventricular tachycardia until conclusively proven otherwise.
Another reason that it is a WCT guideline and not a ventricular tachycardia guideline is because of conditions like WPW (wolff parkinson white syndrome). With WPW, a delta wave may be present causing widening of the QRS complex.
This is important because adenosine, and Cardizem should not be administered to patients with WPW. There is controversy regarding whether Amiodarone is safe with WPW, but as of now the American Heart Association considers it a safe option.
Points to remember:
- O2 & fluids for compensatory tachycardia
- Synchronized cardioversion is the SAFER option
- If QRS is wide treat as V-tach
Recent Posts
Fascicular Tachycardia: how to face it?
Medical Corner - Management of Tachycardiac Arrhythmias in Pregnancy
A successful CPR Saves on a Patient with Refractory Ventricular Fibrillation
Decompensated shock: which are the solutions in emergency?