Internal and external haemorrhoids: causes, symptoms and remedies
Haemorrhoids, about 10% of the adult population in developed countries have suffered from them at least once in their lives
Pain, swelling, a sense of heaviness, itching and in some cases bleeding, this is what haemorrhoids look like
A very frequent pathology at all ages, in both men and women, and which can become an annoying and embarrassing nuisance.
All the more so because until recently surgical treatment was scary.
What are haemorrhoids
Hemorrhoids in the proper sense are not a disease: they are venous pads that we all have straddling the anal orifice and that contribute to the maintenance of its continence.
Hemorrhoidal disease
So it is inaccurate to say ‘I suffer from haemorrhoids'”.
Hemorrhoids are normal veins.
Hemorrhoid disease occurs when these veins become hypertrophied, i.e. swollen, and begin to leak.
This leakage is called prolapse and the annoying symptoms, bleeding and pain begin.
It should be pointed out that haemorrhoidal disease is not a disease of the veins alone, as was thought for a long time, but is also due to degeneration of the connective tissues, which for hereditary or acquired reasons cause the venous cushions to lose support, leading to leakage, i.e. prolapse.
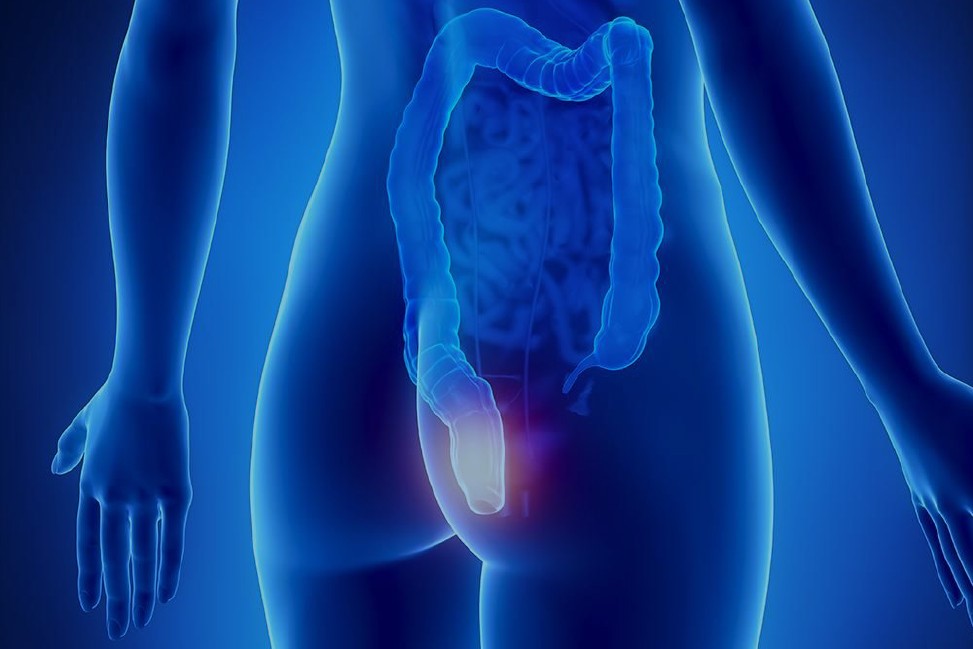
Internal haemorrhoids and external haemorrhoids
There are clinically 2 types of haemorrhoids:
- Internal: located in the anal canal, they are painless and not visible. They can come out during defecation but return spontaneously;
- External: they are visible, develop outside the anal orifice, come out under effort without returning spontaneously or are persistently externalised.
Degrees of haemorrhoids
Hemorrhoids are generally classified according to severity into four grades: from grade one, which is the mildest, where there is only an increase in internal haemorrhoidal congestion, to grade four, which presents an unreducible prolapse with severe inflammation and bleeding.
Hemorrhoids, causes and risk factors
Hemorrhoids occur more frequently in women, as risk factors include pregnancy with increased blood congestion in the pelvis.
Also important are:
- Familiarity;
- constipation;
- lifestyle: unhealthy diet, obesity, sedentarism and type of work (those who are forced to sit for long periods or exert themselves excessively are more at risk).
The symptoms
There are two types of symptoms:
- bleeding: obvious and copious red or even microscopic bleeding, i.e. the patient loses blood in small quantities every day, is not seen and becomes anaemic;.
- pain, which can be of 3 types:
- one is that of congestion, with a feeling of weight, of itching, of burning;
- then a very acute pain when going to the toilet, even unbearable, which indicates that the haemorrhoids are complicated by a fissure;
- finally, the infamous acute attack of haemorrhoids, which occurs when the haemorrhoids prolapse outwards and become swollen, very painful and unrelievable, confining the patient to bed for several days.
These symptoms are often inversely proportional, because if the haemorrhoids bleed they deflate and the more they are deflated, the less they bother you; if the haemorrhoids do not bleed they are more swollen and painful.
How to treat haemorrhoids
The choice of the most appropriate treatment is closely related to the degree of severity of the disease.
If the patient is in an early stage of the disease, it is enough to modify the lifestyle with:
- diet rich in fibre (the Mediterranean diet);
- daily physical activity
- abundant water intake;
- correct intimate hygiene.
There are also trophic drugs based on flavonoids taken by mouth and the classic creams based on local anaesthetics and anti-inflammatory agents that can alleviate the symptoms without, however, acting on the root causes of the problem.
Surgery
When the disease is more advanced (grade III and IV), surgery is the only effective solution.
Until the 1990s, the most common form of surgery was haemorrhoidectomy (Milligan-Morgan operation).
This method solves the problem in a radical way by removing the haemorrhoid nodules, but has a great handicap: the pain, both post-operative and during convalescence.
Hemorrhoidopexy
In 1990 an Italian surgeon, Antonio Longo, proposed a new method of treating the disease, which is based on repositioning the externalised haemorrhoids in their normal location, in the anal canal, thus curing their prolapse, and is called haemorrhoidopexy.
It is an operation performed with mechanical staplers, which remove the prolapse and fix the haemorrhoids inside.
The result is a real lifting of the anal canal: once returned to their normal location, the haemorrhoid pads deflate and stop bleeding and causing pain.
The operation is infinitely less painful in convalescence and minimises the risk of recurrence: it is performed about three centimetres above the anal orifice, where there are no longer any pain fibres.
It is performed as an outpatient surgery, as the patient usually goes home after one day.
Convalescence is very quick: the patient returns to normal life habits at 50-70 per cent after two days, 100 per cent after one week and can do sports after three weeks.
Milligan-Morgan’s surgery was much more painful and the recovery time was one and a half months.
In this field of surgery, too, technological progress has been great in twenty years: today we have new, more effective and safer staplers, which have eliminated the risk of post-operative bleeding and the risk of distant recurrence of haemorrhoidal disease, and in addition, in women they are able to effectively treat the constipation that is often associated with the problem of haemorrhoids: they therefore represent the gold standard for the treatment of this pathology.
Minimally invasive surgery for less severe cases
Finally, in less severe cases where only bleeding prevails, we now have other alternative methods, such as the possibility of ‘deflating’ the venous cushions by locating the small arteries that supply them with blood with an endorectal probe (Doppler), and then ligating them: by closing the taps, the haemorrhoids are decongested and the bleeding stops.
A minimally invasive technique which, in selected cases, gives excellent results, with a hospital stay of just a few hours and an almost painless course.
Read Also:
Secondary Cardiovascular Prevention: Aspirin Cardio Is The First Lifesaver
Sepsis, Why An Infection Is A Danger And A Threat To The Heart


