Measuring performances in prehospital emergency medicine - MEDEST118
SOURCE: MEDEST118, Mario Rugna, MD
 Clinical pathways are the essence of clinical practice. They start from diagnose and therapy (usually provided from a physician) and then continue in assistance (usually provide from a nurse).
Clinical pathways are the essence of clinical practice. They start from diagnose and therapy (usually provided from a physician) and then continue in assistance (usually provide from a nurse).
Medical systems are ensembles of medical professionals, doctors and nurses, and to standardize the diagnose, the therapy and the assistance on every identified clinical pathway a common trace is needed.
Clinical guidelines and evidenced based literature are the bases on whom clinical pathways and best practices are designed. The interventions and the therapies mentioned in clinical guidelines have positive influence on different outcomes so every medical professional can refer to those established common practice to standardize his clinical behavior.
Emergency Medical Systems aim to be considered an excellence in order of clinical, technical and non technical skills. To reach such results financial and human resources are needed. How can we demonstrate that such resources are well invested. In other words which is the impact of emergency medical systems on public health and how can we measure it?
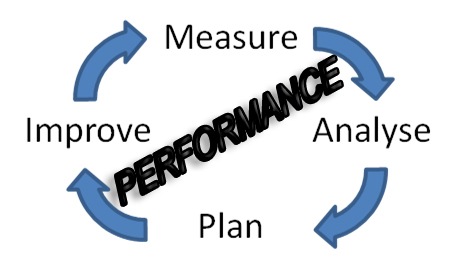
Measuring performances in medicine is an exciting challenge. Pre-hospital emergency medicine and pre-hospital emergency services make no exception. We are the frontline of medical care and beyond organizational duties we have a moral assignment to plan, measure, analyze and improve our performances, both individually and as public system.
First step is to establish a series of Best Practices about a series of representative clinical pathways derived from an epidemiological analysis of our local clinical experience. International guidelines, evidenced based medicine and other forms of medical literature are the field where to find the best interventions and therapies, in term of positive influence on various clinical outcomes, to incorporate in every pathway.
Education, planning and other form of diffusion has to be integral part of the process, to allow the professionals involved to be active part of the story.
The way to define the impact of a medical system on public health is to measure how many of those intended interventions (alone or bundled) will be performed in real practice.
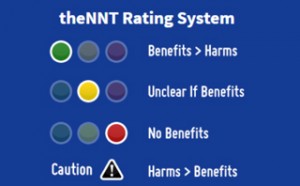 This impact can be expressed in N.N.T. in the contest of every single clinical pathway.
This impact can be expressed in N.N.T. in the contest of every single clinical pathway.
Historically the pre-hospital services where judged on the basis of response times and survival from cardiac arrest, but this new way to measure performance on the base of clinical outcomes is more patient centered and will change the way to analyze the emergency medical systems.
A 5 year experience from Pre-Hospital Outcomes for Evidence-Based Evaluation (PHOEBE) project (the Lincoln Institute for Health), in its impact evaluation says:
“This project will change the way in which the quality of ambulance services is measured. As such, it goes beyond just measuring performance in terms of response times. This may impact on the operation of ambulance services from organisations that concentrate on meeting response time targets towards those that are geared to improving the quality of patient care.”
Let’s make practical examples of combined or single interventions that have decisive impact on public health?
In an article entitled “EVIDENCE-BASED PERFORMANCE MEASURES FOR EMERGENCY MEDICAL SERVICES SYSTEMS:A MODEL FOR EXPANDED EMS BENCHMARKING” published in PREHOSPITAL EMERGENCY CARE 2008;12:141–151 are indicated some clinical pathways to measure in order of NNT
In STEMI patients, according to AHA Guidelines, those three elements make the difference:
-
Aspirin (if not allergic)
-
12-Lead electrocardiograph and pre-arrival activation of interventional cardiology team as indicated
-
Direct transport to percutaneous coronary intervention (PCI) capable facility for ECG to PCI time <90 minutes
When present together (Care Bundle) the NNT is 15 on stroke, 2nd myocardial infarction, or a death. In other terms, every 60 patients that receive the treatment 4 of them avoid the mentioned complications.
Noninvasive positive pressure ventilation (NIPPV) in Pulmonary Edema has a NNT of 6 for need of endotracheal intubation (ETI). In other terms every 6 NIPPV applied in pulmonary edema patients 1 ETI is avoided.
And so on for other pathways…..
Recently Care Flight a Medical retrieval service based in Australia posted on its blogsite The Collective a post on this topic entitled PHARM quality – how do you know when you’re doing it well?
In this post Dr. Alan Garner talks about Carebundle approach (here the definition from Institute for Healthcare Improvement (IHI) website) to track performances in EM.
He also mentioned how German based company ADAC use this method (defined as “tracer diagnosis” by Erwin Stolpe chair of the ADAC medical committee) to report performances on defined clinical pathways.
And here some resources from Erwin Stolpe
I think that, as in hospital, prehospital emergency environment has to report and track performance quality to improve and justify the investment of financial and human resources.
Every medical system has to target the right method to his particular logistic and cultural situation, but has to find a way to measure how good it is and how good its professionals works.
This gonna take us out from sterile discussion about which is the best model in prehospital emergency medicine and let’s us to make a step forward to demonstrate which organizational model really works in term of public health and patients centered clinical outcomes.


