Toxic shock syndrome in emergencies: what is it?
Toxic shock syndrome is a clinical condition characterised by the rapid onset of fever, skin rash, low blood pressure and muscle pain
It is mainly caused by substances, called toxins, produced by bacteria such as staphylococci, which are capable of causing a major inflammatory reaction throughout the body.
The onset of symptoms of toxic shock syndrome is sudden, with:
- Fever;
- Chills;
- Generalised malaise;
- Weakness;
- Headaches;
- Sore throat;
- Muscle aches and pains;
- Abdominal pain;
- Vomiting and diarrhoea;
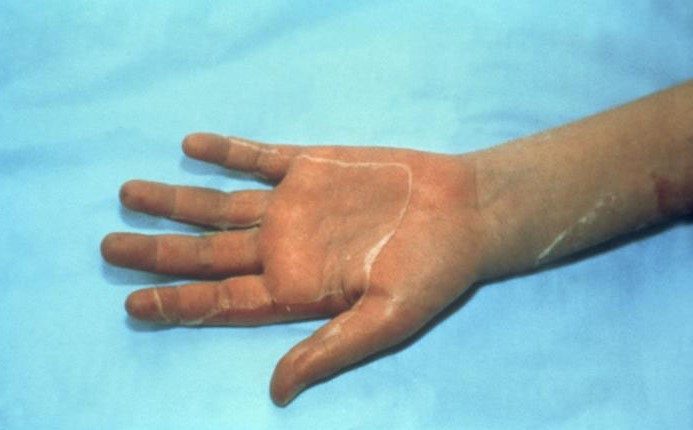
- Appearance within 24 hours of diffuse and uniform reddening of the skin followed by desquamation.
Within 3 to 7 days of onset, flaking affects the palms of the hands and soles of the feet.
The general condition may progressively worsen with multi-organ involvement characterised by the appearance of:
- Low blood pressure;
- renal failure with reduced urine elimination;
- Liver failure;
- Low platelet count;
- Poor blood flow to the brain, which may manifest as drowsiness, confusion, irritability, agitation and hallucinations.
The diagnosis of toxic shock syndrome should be suspected in healthy children in whom the sudden onset of fever, rash, low blood pressure and multi-organ suffering is observed
Risk factors include:
- In post-pubescent adolescents by the use of internal tampons;
- history of recent surgery;
- recent infections of skin and soft tissues, the most superficial parts of the body.
The diagnosis of toxic shock syndrome is based on clinical criteria: fever, low blood pressure, diffuse erythema and scaling with involvement of at least three organs and/or apparatuses.
It must be demonstrated by blood tests and cultures that the illness is not caused by an infection.
Blood, tissue or vaginal cultures in menstruating girls should always be obtained, but isolation of Staphylococcus is not necessary for diagnosis: isolation of the bacterium is observed in only 5% of cases.
Continuous monitoring of the function of the kidney, liver, bone marrow, heart and lungs is essential.
Instrumental investigations (MRI and CT) are necessary in case of ischaemia or cerebral oedema.
Toxic-Shock-like Syndrome or Streptococcal Toxic Shock Syndrome (STSS) is a variant very similar to Toxic Shock Syndrome (TSS)
It is caused by the type A erythrogenic toxin produced by a type of Streptococcus, beta haemolytic A (SBEA). The gateway is usually a rapidly spreading skin infection.
Streptococcal toxic shock syndrome most frequently causes soft tissue cell death, generalised erythematous-maculo-papular rash, blood clotting problems and liver damage, whereas staphylococcal toxic shock syndrome most frequently causes vomiting, diarrhoea, diffuse scarlet rash, mucosal redness, mental confusion, thrombocytopenia.
Kawasaki disease has several features in common with toxic shock syndrome but is usually less severe
Both are associated with fever that does not abate with antibiotic therapy, reddening of the mucous membranes and erythematous rash and associated scaling.
Many symptoms of toxic shock s. are however rare or absent in Kawasaki disease including diffuse muscle pain, vomiting, abdominal pain, diarrhoea, low blood pressure and shock.
COVID-19-related paediatric multi-system inflammatory syndrome:
Multi-organ inflammatory syndrome characterised by fever, shock, inflammation of the heart muscle (myocarditis), abdominal pain, clinical picture similar to Kawasaki disease.
Positive tests for COVID-19 have been observed in some, but not all, patients with this clinical syndrome.
Rocky Mountain Fever:
Caused by Rickettsia rickettsii, it is transmitted by ixodidae ticks.
The basic symptoms are high fever, severe headache and rash.
Patients with suspected toxic shock s. should be immediately admitted to intensive care for supportive therapy with intravenous infusion and vasopressors to aid blood circulation, and possibly with intubation and assisted ventilation.
Treatment with intravenous antibiotics is highly recommended for all patients.
Antibiotic therapy should be prolonged until the patient no longer has a fever, usually after 10-14 days.
In severe cases of toxic staphylococcal shock syndrome that have not resolved with fluid and vasopressor drugs, intravenous immunoglobulin therapy is recommended.
Corticosteroids are not recommended.
Read Also:
Intraosseous Access, A Life-Saving Technique In Emergency Shock Management



