Traumatic pneumothorax: symptoms, diagnosis and treatment
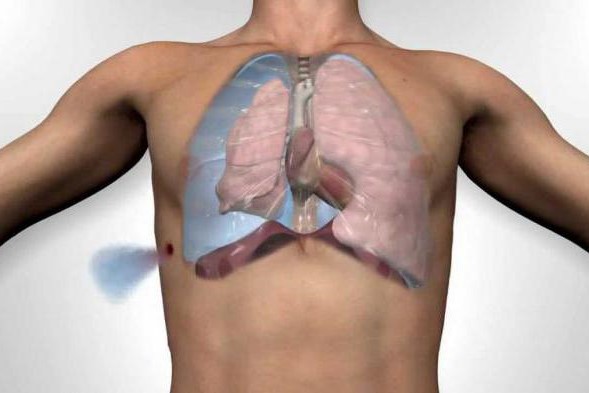
Traumatic pneumothorax is the presence of air in the pleural space as a result of trauma, causing partial or complete collapse of the lung
Symptoms include chest pain caused by the injury and sometimes dyspnoea. The diagnosis is made by chest X-ray.
Traumatic pneumothorax, usually treated with chest drainage
Pneumothorax may be caused by blunt or penetrating trauma; many patients also have a haemothorax (haemopneumothorax).
In patients with penetrating wounds through the mediastinum (e.g., medial wounds to the nipples or scapulae), or with severe blunt trauma, a pneumothorax may be caused by rupture of the tracheobronchial tree.
Air from the pneumothorax may enter the soft tissues of the chest and/or neck (subcutaneous emphysema), or the mediastinum (pneumomediastinum).
A simple unilateral pneumothorax, even a large one, is well tolerated by most patients unless they have significant underlying lung disease.
However, an overstretched pneumothorax may cause severe hypotension, and an open pneumothorax may compromise ventilation.
Symptomatology of traumatic pneumothorax
Patients with traumatic pneumothorax commonly have pleuritic chest pain, dyspnoea, tachypnoea and tachycardia.
Breathing sounds may be diminished and the affected haemithorax hypertympanic on percussion, particularly in extensive pneumothoraces.
However, these findings are not always present and may be difficult to detect in the noisy resuscitation setting.
Subcutaneous emphysema causes a crackling or creaking sound on palpation; findings may be localised to a small area or cover a large portion of the chest wall and/or extend to the neck; extensive involvement suggests rupture of the tracheobronchial tree.
Air in the mediastinum may produce a characteristic creaking sound synchronous with the heartbeat (Hamman’s sign or Hamman’s crunch), but this sign is not always present and is also occasionally caused by injury to the oesophagus.
Traumatic pneumothorax, diagnosis
- Chest X-ray
The diagnosis is usually made by chest X-ray.
Ultrasonography (done at the patient’s bedside during initial resuscitation) and CT scan are more sensitive for small pneumothoraces than chest X-ray.
The size of a pneumothorax, determined by the percentage of the hemithorax that is empty, can be estimated from the radiological findings.
The numerically expressed size is valuable primarily for quantifying progression and resolution, rather than for determining prognosis.
Treatment
- Usually thoracostomy tube
The treatment of most pneumothoraces is with insertion of a chest drain (e.g., 28 Fr) into the 5 or 6 intercostal space anterior to the mid axillary line.
Patients with small pneumothoraces and no respiratory symptoms can simply be observed with a series of chest X-rays until the lung re-expands. Alternatively, a small draining pigtail catheter may be placed.
However, chest drainage should be placed in patients who are to be placed under general anaesthesia, positive pressure ventilation, and/or airway, as these interventions may convert a small, simple (uncomplicated) pneumothorax into a hypertensive pneumothorax.
If a large air leak persists after chest drainage, tracheobronchial lesions should be suspected and bronchoscopy or immediate surgical consultation should be arranged.
Read Also:
Tracheal Intubation: When, How And Why To Create An Artificial Airway For The Patient
What Is Transient Tachypnoea Of The Newborn, Or Neonatal Wet Lung Syndrome?



