Acute and chronic sinusitis: symptoms and remedies
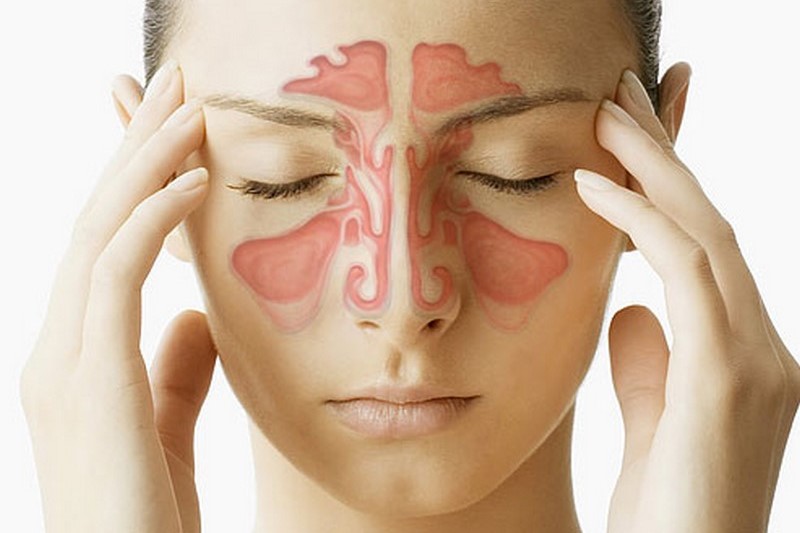
What is sinusitis? Often confused with the common cold due to very similar symptoms, sinusitis is a state of inflammation of the mucous membranes located below the facial sinuses, usually caused by bacteria, more rarely by viruses and fungi (e.g. in some people with a debilitated immune system or in allergic individuals)
In general, one speaks of rhinosinusitis because the nasal cavity system proper and the paranasal sinuses form a single system.
Conditions conducive to the development of sinusitis include the condition of the ostium-meatal complexes, i.e. the passage and drainage point between the sinus cavities and paranasal sinuses.
Factors favouring the onset of the process include anatomical conditions that alter the passage of air currents within the nose or functional factors such as an allergic rhinopathy or cellular rhinitis (NARES, NARESMA), in which the presence of certain cells in the nose such as mast cells and/or eosinophils and the factors they release lead to a state of chronic tissue imbibition that hinders drainage, can lead to polyposis and sinus stagnation, which then turns into sinusitis.
Another contributory cofactor may be a reduction in ciliary mucus transport, a cleansing system of the naso-sinus cavities that may be reduced by exposure to irritants, cigarette smoke or living in poorly humidified environments. Rarely, there may be a congenital defect of ciliary motility.
Sinusitis is called acute if it lasts three to four weeks, subcute if it lasts about 1-3 months, chronic if it lasts longer
When a person suffers from sinusitis, the normal flow of mucus from the facial sinuses to the back of the throat is interrupted, the mucous membranes swell and the mucus becomes trapped within the sinuses themselves and becomes denser, has a greenish-yellow colour and becomes frankly purulent. This accumulation of mucus is the ideal prerequisite for the reproduction of fungi and bacteria.
Causes and risk factors of sinusitis
People with nasal defects (presence of polyps, deviated nasal septum, facial tumours, but also abuse of decongestants) have a higher than standard risk factor of contracting sinusitis.
Signs and symptoms of sinusitis
The typical symptoms of sinusitis are nasal congestion with obstruction, coughing, fever, emission of greenish mucus, toothache and headache; if chronic, the discharge of pus in the back of the pharynx may give halitosis, serous mucous or purulent otitis may also be associated due to obstruction of the normal functioning of the Eustachian tube and alterations in middle ear ventilation.
In addition, pulmonary symptoms such as bronchospasm ect (rhino bronchial syndrome) may be associated in predisposed individuals.
Sinusitis is often confused with rhinitis due to the similarity of the presenting symptoms; in this case, however, the secretion is not purulent but mucous or frankly serous like water in allergic and cellular rhinitis associated with sneezing and nasal itching.
Possible complications of sinusitis are degeneration into chronic sinusitis, formation of abscesses, bacterial resistance to antibiotics, osteomyelitis, a thrombosis or thrombophlebitis of the cranial.venous sinuses.
How to prevent sinusitis
Preventing sinusitis is basically based on treating allergies (many allergy sufferers are prone to sinusitis), cellular rhinitis diagnosed by nasal cytology, upper airway infections, abstaining from smoking, staying in temperatures that are too hot or too cold or too dry, and avoiding contact with pollutants.
The use of decongestants in upper airway infections can reduce the risk of sinusitis; however, it should be remembered that these products can be addictive, so they should be used sparingly
Diagnosis of sinusitis
The diagnosis of sinusitis is usually already made by the family doctor and is essentially based on an interview with the patient regarding symptoms and a physical examination of the throat, nose and facial sinuses.
It must be taken into account that some facial aches and pains may be of pastural origin, so not always a frontal pain may be related to a sinusopathy, but also an ocular problem, a contraction of the postural musculature.
A clinical and anamnesis and an ENT examination with endoscopic evaluation of the nose always count
This is to avoid unnecessary antibiotic treatment.
If necessary, the diagnosis may be confirmed by a CT scan of the facial sinuses in cases where the symptoms are not indicative of the disease; it will be mandatory if antibiotic therapy has had no effect or if the sinusitis has lasted for more than eight weeks.
Other examinations that can help make the diagnosis are endoscopy, radiography, ultrasonography, transillumination, mucus culture and biopsy.
Mucus culture highlights the type of micro-organism present in this secretion and thus allows the doctor to prescribe the appropriate antibiotic therapy to eliminate just that type of bacterium.
Mucus samples are taken from the nose, not from the sinuses, although it may happen that the micro-organisms present in the mucus are different from those in the sinuses.
For this reason, it may sometimes be necessary to use an invasive method of analysis to take mucus (or sometimes pus or other secretions) directly from the frontal sinuses.
If, on the other hand, the sinusitis is of fungal origin, then surgery will be necessary to make the diagnosis and prepare the appropriate therapy, since fungi are not to be treated with antibiotics, but with antifungal drugs.
The danger of fungal sinusitis is mainly related to the danger that the micro-organism that caused it may have penetrated into the bone.
In this case, only a bone biopsy can determine whether this infiltration has occurred.
With a biopsy, a piece of tissue is taken by inserting a flexible instrument into the nose.
Biopsy is also used to diagnose other causes of sinusitis, such as motionless cilia syndrome.
Although to check for ciliary movement it is sufficient to cool a mucus sample with physiological saline on a slide and observe it with a phase-contrast microscope, this is a simple assessment that all practitioners doing outpatient nasal cytology can do.
Sinusitis therapy
The aims of treatment are to cure the underlying infection and improve symptoms.
Antibiotics are the therapy of choice for sinusitis of bacterial origin, combined with nasal lavage and local medical therapy.
The therapy must always be completed, without discontinuing it as soon as improvement is noticed, otherwise the treatment will have no effect, and may even induce antibiotic resistance in the patient.
To relieve symptoms, the use of decongestants and mucolytics can help to rid the sinuses of excess mucus.
If antibiotic therapy does not yield the desired results, surgery may be necessary.
Surgery is the only treatment for those with nasal defects such as septal deviation or the presence of polyps, but also in cases of sinusitis of fungal origin.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Vancomycin-Sensitive Staphylococcus Infections: Symptoms And Treatment
Pneumococcal Vaccine: What It Is And How It Works
Sinusitis: How To Recognise That Headache Coming From The Nose
Sinusitis: How To Recognise And Treat It
Flu Vaccine For Children? Paediatricians: ‘Do It Now, Epidemic Already Started’


