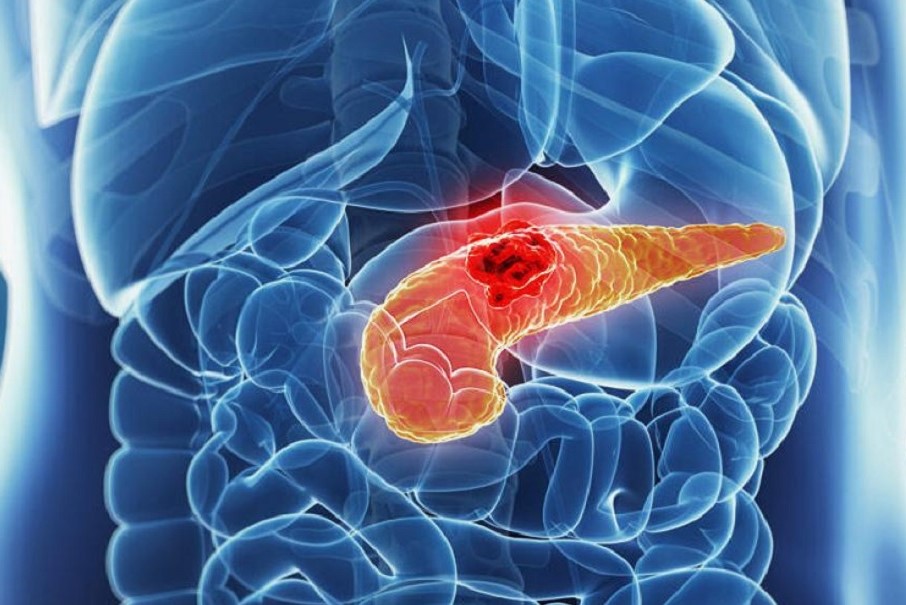
Acute pancreatitis: causes, symptoms, diagnosis and treatment
Acute pancreatitis is an inflammation of the pancreas with a sudden onset, the most common cause of which is biliary stones
Acute pancreatitis can be mild or severe and is manifested by severe pain in the abdomen.
What is acute pancreatitis?
Acute pancreatitis is an inflammation of the pancreas that occurs suddenly.
The pathological picture is very variable and can present with mild forms of pancreatitis, which resolve within a few days, and more severe forms, which can even be fatal.
What are the causes of acute pancreatitis?
Pancreatitis most frequently arises as a result of biliary stones, a condition that most frequently affects women.
Alcoholism, which affects men more frequently, is also a risk factor that can facilitate the onset of pancreatitis.
Anatomical abnormalities of the pancreas, tumours, increased triglycerides in the blood or the intake of certain drugs can also cause the onset of the disease.
Acute pancreatitis can also be a complication of endoscopic manoeuvres on the pancreas.
What are the symptoms of acute pancreatitis?
Acute pancreatitis is most frequently manifested by significant abdominal pain that is often associated with nausea, vomiting and fever.
In milder forms of pancreatitis, the symptoms may rapidly regress, while in more severe forms, they may evolve into septicaemia, shock, renal and respiratory failure.
Diagnosis
The painful symptoms experienced by the patient allow the specialist to orientate the diagnosis: pain in the upper abdomen (rod-like) is very common and can also spread to the back (belt-like).
Blood tests can be used to check whether the values of certain enzymes (amylase and lipase) have risen; the pancreas physiologically produces these enzymes, but if the pancreatic tissue is damaged, these substances pass into the bloodstream and increased values are therefore recorded in the blood.
It is important for the specialist to recognise severe forms of acute pancreatitis at an early stage, because in these cases it is necessary to intervene on the patient in a targeted and immediate manner.
Other blood tests and a CT scan of the abdomen, performed with contrast medium, make it possible to distinguish mild from severe forms at the diagnosis stage.
An ultrasound scan can be used to check for gallstones, which are the most common cause of pancreatitis.
Treating acute pancreatitis
Acute pancreatitis rarely requires urgent surgical intervention.
If gallstones are the cause of the condition, the patient will undergo cholecystectomy surgery (removal of the gallbladder), usually performed laparoscopically.
Treatment for acute pancreatitis initially involves fasting and intravenous administration of fluids and electrolytes.
Patients with more severe forms will also be prescribed antiproteasic drugs and antibiotics.
Mild forms (about 90% of the total) usually resolve within 7-15 days, leaving no trace.
More severe forms, on the other hand, which may require several surgical interventions, have a mortality rate of 10-20%.
In these cases, surgery is very difficult and is aimed at draining the intra-abscesses that form in the pancreas and the infected and necrotic pancreatic tissue.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Gestational Diabetes, What It Is And How To Deal With It
Pancreatic Cancer, A New Pharmacological Approach To Reduce Its Progression
What Is Pancreatitis And What Are The Symptoms?
Kidney Stones: What They Are, How To Treat Them


