Lipid profile: what it is and what it is for
Several lipid profile parameters can be determined in the laboratory. These values have different meanings, and the same indications do not apply to all of them
Total lipids
Their determination is useless, since no clinical decision can be made on the basis of this parameter.
Which tests define the lipid profile
Lipidogram
Separation of plasma lipoprotein classes by electrophoresis or ultracentrifugation makes it possible to identify chylomicrons, slow-moving betalipoproteins (LDL), fast-moving alphalipoproteins (HDL) and intermediate-moving pre-betalipoproteins (VLDL).
This examination, which forms the basis of the Fredrickson classification of hyperlipidemias, does not allow differentiation between primary and secondary forms and is not relevant for therapy in the vast majority of cases.
For these reasons, the lipidogram is never a primary examination and should be reserved for the study of selected patients with severe dyslipidaemia.
A balanced diet should be observed for a fortnight prior to sampling.
Avoid ingesting alcohol 24 hours before the test.
Fasting for 12 hours prior to blood sampling.
Cholesterol
This is a first level test.
The proportional correlation between cholesterolaemia and ischaemic heart disease is proven.
Fasting is not required for its determination.
Cholesterolaemia increases with age, reaching a fairly stable value around the age of 60 in males, while in women it increases further.
The reference limits provided by laboratories should be related to age and sex (in any case, the desirable cholesterolaemia is up to 180 up to the age of 30, up to 200 for all other ages); many reports, however, do not express different ranges for age and sex, but an ‘ideal’ or a ‘minimum acceptable’ value.
Beyond the age of 65, the prognostic value of cholesterol is controversial.
Cholesterol is introduced daily through the diet (exogenous share) but is also synthesised by liver cells and practically every cell in the body (endogenous share).
It is increased in cholesteryl ester storage disease, polygenic hypercholesterolaemia, multiple familial hyperlipidaemia, hypothyroidism, nephrotic syndrome, dysglobulinemia, cholestatic jaundice, Cushing’s disease, diabetes mellitus, acute itermitting porphyria, chronic pancreatitis, glomerulonephritis.
It is decreased in alpha-lipoprotein deficiency, hyperthyroidism, liver failure, anaemia, cachexia, malnutrition, uremia, Addison’s disease.
Medications such as ACTH, corticosteroids, androgens, bile salts, catecholamines, phenothiazines, oral contraceptives, thiouracils may raise blood levels.
Patients should refrain from drinking alcoholic beverages 24 hours and eating food 12 hours before the test.
Triglycerides
The correlation between hypertriglyceridemia and increased coronary risk is not clearly established.
The triglyceride assay is necessary to calculate the LDL fraction; it undergoes considerable intra-individual variation in relation to diet and alcohol intake and should be determined after a 12-hour fast.
Very high triglyceride levels (>1,000) carry a high risk of pancreatitis.
Triglycerides are increased due to exogenous causes, from excessive intake of alcohol, carbohydrates and lipids.
They are also increased by familial lipoprotein lipase deficiency, a congenital disease evident early in life and familial endogenous, autosomal dominant disease with increased VLDL.
Alcohol, cholestyramine, corticosteroids, cholestipol, oral contraceptives, thyroid preparations, oestrogens, furosemide, miconazole can increase blood values of triglycerides.
Clofibrates, heparin, pergonal, androgens, niacin, anabolic steroids and ascorbic acid decrease triglyceride levels.
Abstain from drinking alcohol 24 hours before and food 12 hours before the test.
Discontinue any interfering drug therapy.
HDL cholesterol
It is contained in high-density lipoproteins.
It is decreased in diabetes mellitus, hyperlipoprotein type IV, nephropathy, hepatopathy.
Its decrease is an atherogenic risk factor (myocardial infarction, cerebral, peripheral vasculopathies).
A high concentration (> 60 mg/dl) is considered protective, while values below 45 mg/dl are considered an independent cardiovascular risk factor.
Abolishing smoking and increasing physical activity increase the HDL fraction.
The HDL assay is necessary for calculating the LDL fraction.
When the triglyceride value is above 400 mg/dl, HDL cholesterol determination by common methods is unreliable and must be performed in specialised centres.
It is increased during therapy with oral contraceptives, insulin, ACTH, hydantoin, clofibrate, vitamin C.
A balanced diet should be observed for a fortnight before the test.
Avoid ingesting alcohol 24 hours before the test.
Fasting during the 12 hours before the test.
LDL-Cholesterol
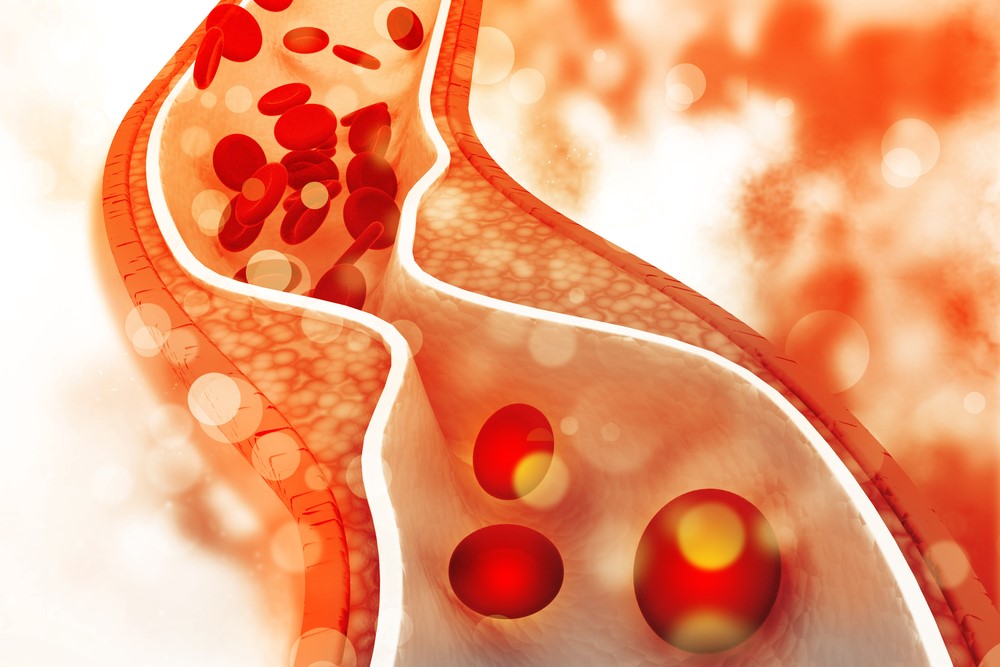
This is the fraction of cholesterol bound to low-density proteins.
It is the atherogenic fraction of cholesterol.
In American guidelines and more recent trials, its value is taken as a reference point for discriminating the ‘threshold’ for drug therapy.
If triglycerides are normal or 400 mg/dl, there is no need to measure it as its value can be calculated using the Friedewald formula:
LDL = total cholesterol ? (HDL + 1/5 triglycerides)
When the triglyceride value exceeds 400 mg/dl, the Friedewald formula is unreliable and it is therefore necessary to determine LDL-cholesterol using ultracentrifugation methods; in this case, the patient must remain fasting.
A balanced diet should be observed for a fortnight prior to sampling.
Avoid ingesting alcohol 24 hours before the test. Fasting for 12 hours prior to blood sampling.
Plasma apolipoproteins (A, B, E)
These are glycoproteins that transport plasma lipids in the circulation and are involved in lipoprotein synthesis and catabolism processes.
APO-A are the protein carrier of HDL, APO-B are prevalent in LDL and VLDL.
Plasma apolipoproteins.
The determination of apo A and E is further along in standardisation than that of total cholesterol and HDL.
However, many are reluctant to use it because after all, apo A1 information is equal to that of HDL cholesterol, and apo B information is equal to that of LDL cholesterol.
In addition, treatment guidelines are targeted at LDL-cholesterol.
The ideal lipid profile
Plasma lipid levels vary significantly in different populations depending on genetic as well as environmental factors, particularly diet.
It is therefore difficult to define ‘normal’ values; rather, the large trials conducted in recent years and the various international organisations and study groups have identified ‘acceptable’ values insofar as they correlate with a lower cardiovascular risk and are therefore ‘desirable’, and values above which the risk progressively increases from moderate to high.
The definition of these limits is of fundamental importance in deciding the subsequent diagnostic and therapeutic strategy.
Values of total cholesterol below 200 mg/dl and LDL-cholesterol below 130 mg/dl are ‘desirable’.
Limit’ values for total cholesterol are considered to be between 200 and 239 mg/dl and for LDL-cholesterol between 130 and 159 mg/dl.
Values above these are defined as ‘high’ and are associated with a high risk of developing ischaemic heart disease.
Recently, the American Heart Association Task Force on Risk Reduction reinforced the importance of defining HDL-cholesterol and triglyceride levels in the routine assessment of the lipid picture; they should, if necessary, be modified to achieve an improvement in the risk profile.
HDL-cholesterol values between 40 and 50 mg/dl in men and 50 and 60 mg/dl in women are ‘desirable’; for triglycerides, values below 200 mg/dl are ‘desirable’, values between 200 and 400 mg/dl are ‘borderline’ and values above 400 mg/dl are ‘high’.
Lipid profile: the cholesterol self-analysis
Self-analysis of plasma cholesterol can be performed in certain pharmacies with an enzymatic method that only requires capillary fingertip sampling.
Enzymatic reagents and a special reader are used.
In order to obtain an analytically reliable data, however, it is advisable to go to an analysis laboratory with venous sampling.
It is necessary to abstain from alcohol for 72 hours and food for 12 hours before taking the sample. The quantity required for analysis is a single drop of blood.
Adults (40-60 years of age) and obese and/or at-risk individuals should have their cholesterol analysed at certain intervals.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
What Is Albumin? Tests For Measuring Liver And Kidney Function
Defibrillator: What It Is, How It Works, Price, Voltage, Manual And External
The Patient’s ECG: How To Read An Electrocardiogram In A Simple Way
Signs And Symptoms Of Sudden Cardiac Arrest: How To Tell If Someone Needs CPR
Inflammations Of The Heart: Myocarditis, Infective Endocarditis And Pericarditis
Quickly Finding – And Treating – The Cause Of A Stroke May Prevent More: New Guidelines
Atrial Fibrillation: Symptoms To Watch Out For
Ischaemic Heart Disease: What It Is, How To Prevent It And How To Treat It
Family Hypercholesterolemia: What It Is And How To Treat It
What Is Cholesterol And Why Is It Tested To Quantify The Level Of (Total) Cholesterol In The Blood?


