Surgical interventions: what is minimally invasive vitrectomy?
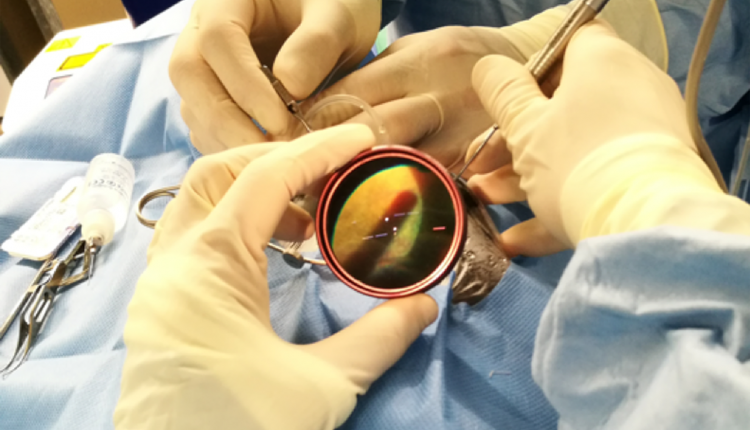
Vitrectomy is a surgery of the posterior segment of the eyeball (vitreous cavity) that consists of the removal of the vitreous gel
Originally, the technique involved cutting and opening the conjunctiva and opening the sclera to enter the vitreous cavity, then the conjunctiva and sclera were sutured with resorbable stitches.
Thanks to the technological development of small-calibre instruments, minimally invasive vitrectomy retains the same capabilities and allows the creation of self-sealing 0.5 millimetre incisions, which do not require sutures.
What is minimally invasive vitrectomy?
The indications for minimally invasive vitrectomy are diverse, and today practically all operations of the posterior ocular segment can be performed using this technique.
In the application of this technological development our retina surgeons are pioneers in Italy.
The indications are:
- Retinal detachment, simple or complicated by proliferations
- Diabetic retinopathy with or without retinal detachment
- Epiretinal membrane or macular pucker
- Complete macular hole or pseudo-hole
- Vitreous opacity related to bleeding or inflammatory problems
- Uveitis
- As a tool to diagnose rare diseases of the posterior segment
What are the advantages and disadvantages of minimally invasive vitrectomy?
The procedure is performed through very small incisions that do not require sutures.
This results in a faster functional recovery with less intraocular inflammation.
Patients also complain of less discomfort than with conventional surgery.
The safety of the technique has been validated in several clinical studies, demonstrating a safety profile equal or superior to the traditional technique.
Minimally invasive vitrectomy is also accompanied by a change in the type of anaesthesia, as general anaesthesia has been replaced by loco-regional anaesthesia.
More than 90% of the vitrectomies in our centre are performed under loco-regional anaesthesia, which blocks the movement and sensitivity of the eyeball and together with careful sedation of the patient makes the procedure much more tolerable for the patient.
The change in anaesthesia has improved patient comfort and at the same time reduced the potential serious risks of a general anaesthesia, also limiting the time spent in hospital.
Are there any rules for preparing for surgery?
Based on an accurate diagnosis, patients with retinal surgery are followed up in specific outpatient clinics run by our surgeons.
When the indication for surgery is given, the patient is informed about the type of surgery he will undergo to solve his problem, and whether the surgery will be carried out in the DAY HOSPITAL.
The patient will have to wait for a call from the secretaries of the Ophthalmology Unit, who will schedule all the necessary pre-admission examinations (blood tests, examination by the anaesthetist and possibly by the cardiologist or diabetologist). A date for the operation will then be decided.
The treatment after the operation is decided by the surgeon, depending on the type of surgery performed.
As a general rule, all patients will have to take oral antibiotics for the first 4 days after surgery and antibiotic anti-inflammatory eye drops for about 1 month after surgery.
The surgeon will sometimes use endocular tamponades.
If gas or a type of silicone oil is used, the patient will have to maintain a special positioning, for the first few days after surgery, according to the surgeon’s instructions to help the retina heal properly.
Follow-up
Once the operation has been performed, all patients are seen on the first day, at one week, at one month and at the third month in the specific outpatient clinics for vitreo-retinal diseases, so that the course of treatment is closely followed by the vitreo-retinal surgeons themselves.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Autoimmune Diseases: The Sand In The Eyes Of Sjögren’s Syndrome
Blepharoptosis: Getting To Know Eyelid Drooping



