Treatment and Prognosis of Mediastinitis: what are mediastinal infections?
Mediastinal infections (jointly referred to as mediastinitis) are primarily related to surgery, perforation of the esophagus and infectious spread from adjacent regions, with incidence varying by clinical setting. Postoperative mediastinitis is the most frequently observed entity.
When confronted with acute mediastinitis, all treatment endeavors should be tailored to the primary pathology and associated clinical manifestations
While surgery is often pursued in acute cases of the disease, in chronic cases the utility of surgical treatment is merely palliative.
In general, a multidisciplinary specialist approach is warranted, considering both the overall patients’ condition and the specific disease dynamics and characteristics that resulted in mediastinitis in the first place.
Early diagnosis, definitive initial therapy and scheduled computed tomography follow-up after initial treatment are needed to assess the need for surgical re-intervention.
General principles of mediastinitis management
Even though the management of mediastinitis is guided by the underlying disease etiology, certain elements of care are common to all patients. As a rather severe infection, mediastinitis often advances into septic shock.
In patients with descending necrotizing mediastinitis, there is a strong correlation between the time of admission to the intensive care units (and pertaining severity scores) and overall mortality.
A compromised airway should be expected early in the course of management, especially in cases that are known to involve the neck and upper part of the mediastinum.
Due to local swelling and lockjaw, frontal access to the airway and laryngoscopic visualization may be compromised.
Expert guidelines stipulate that the anesthesiologist should manage the airway (with a well-delineated alternative plan).
However, the involvement of both maxillo-facial surgeon and otolaryngologist during the intubation planning process is endorsed, but also their presence at the time of intubation to mitigate the potential difficulties.
Antimicrobial treatment
When antimicrobial treatment of mediastinitis is considered, it should be guided under the same principles akin to empirical antimicrobial therapy in patients admitted to the intensive care unit.
However, microbiological samples have to be collected before antibiotics are started.
As specific data on the efficacy of antibiotics in mediastinitis are scarce, current recommendations are still mostly based on expert opinion.
In mediastinitis caused by deep sternal wound infection, empirical antimicrobial treatment has to cover methicillin-susceptible Staphylococcus aureus, Gram-negative bacteria of gastrointestinal origin and skin commensal bacteria. Broad-spectrum beta-lactam penicillin is usually prescribed.
Patients presenting with mediastinitis due to esophageal perforation usually receive broad-spectrum antimicrobial agents intravenously that cover aerobic and anaerobic bacterial species that reside in the upper gastrointestinal tract.
Drugs of choice include third-generation cephalosporins (usually with the addition of metronidazole).
Finally, in mediastinitis that arises due to descending necrotizing mediastinitis, empirical treatment has to cover aerobic and anaerobic bacteria associated with infections of the ear, nose, and throat.
A similar scheme to the aforementioned approach in esophageal perforation is recommended, usually with the addition of clindamycin.
Mediastinitis, surgical approaches
Controlling the infectious source and tissue debridement (when necessary) are two fundamental steps in the surgical treatment of mediastinitis.
The strategy is decided according to the underlying cause and magnitude of the disease.
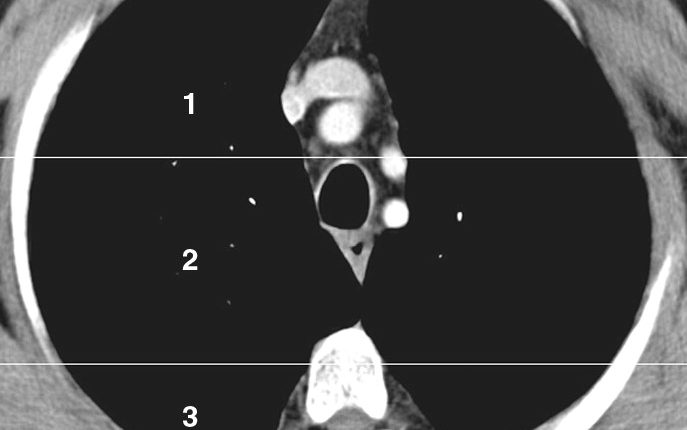
This is usually established with the use of imaging techniques, more specifically cross-sectional imaging studies.
When mediastinitis is situated in the upper part of the mediastinum, it is usually sufficient to conduct transcervical drainage; on the other hand, cases of the disease extending below the tracheal carina (ridge separating the openings of two main bronchi) usually necessitate cervical/transthoracic drainage.
It has to be emphasized that a delay between diagnosing the condition and surgical intervention is linked to poorer outcomes and, therefore, this period should not be longer than 24 hours.
Prevention of mediastinitis
A myriad of preventative measures is effective for reducing the incidence of mediastinitis.
Most of them are in line with basic measures that are used to prevent surgical site infections – most notably preoperative screening to exclude the carriage of multidrug-resistant microorganisms.
Naturally, strict adherence to aseptic techniques during surgery, antimicrobial prophylaxis, appropriate hemostasis, precise surgical technique, careful sternal closure, and adequate wound management are all pivotal for preventing the rise of mediastinitis, with all its potential dire consequences.
Author of the article: Dr. Tomislav Meštrović / News-Medical
Read Also:
What To Know About The Neck Trauma In Emergency? Basics, Signs And Treatments
XStat Hemostatic Device, One Of The Top 10 Best Invetion In 2014
Sources:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1312210/
https://academic.oup.com/ejcts/article/51/1/10/2670570
https://onlinelibrary.wiley.com/doi/abs/10.1002/hed.24183
https://link.springer.com/article/10.1007%2Fs00104-016-0172-7
https://www.clinicalmicrobiologyandinfection.com/article/S1198-743X(19)30394-5/fulltext
Rees CJ, Cantor RM, Pollack Jr. CV, Riese VG. Mediastinitis. In: Pollack Jr. CV (eds) Differential Diagnosis of Cardiopulmonary Disease. Springer, Cham, Springer Nature Switzerland AG 2019



