Persistent Leg drainage in a paediatric trauma patient: case report on a 7-year-old child
Persistent Leg drainage in a paediatric trauma patient: a 7-year-old male with a past medical history of asthma sustained multiple injuries in a motor vehicle accident including a left hip dislocation, left femur fracture, left radial fracture, a comminuted fracture of the lateral wall of the right orbit, a right retrobulbar hemorrhage and a non-displaced fracture of the posterior wall of the right maxillary sinus
Drainage in a paediatric trauma patient, presentation of the case report
He underwent closed reduction of the left hip dislocation, external fixation of the left femur fracture and closed reduction and casting of the left radial fracture with removal of the external fixator and submuscular plating of the left femur 7 days later.
He was initially lost to follow-up until a visiting nurse, caring for his mother, noted that his left femur wound was draining.
At his orthopedic visit 4 months after his accident, his physical examination was significant for a purulent collection at one of his incisions on the left lateral thigh.
The rest of his physical examination was normal, and he was admitted to the hospital for further workup.
The purulent collection was aspirated and was ultimately culture negative.
A radiograph of the left femur showed exuberant callus at the fracture sites.
His vital signs included a temperature of 36.9 °C, pulse of 118 beats/min, blood pressure of 105/47 mm Hg, respiratory rate of 20 breaths/min and oxygen saturation of 100% in ambient air.
His laboratory studies on admission were: white blood cell count of 14.9 × 1000/μL (reference range 4.0–15.0 × 1000/μL) with 69.9% neutrophils (reference range 26.0%–77.0%), 17.3% lymphocytes (reference range 12.0%–60.0%), 8.9% monocytes (reference range 3.0%–14.0%), 3% eosinophils (reference range 0.0%–10.0%), 0.2% basophils (reference range 0.0%–4.0%) and 0.7% immature granulocytes (reference range 0.0%–3.0%), high sensitivity C-reactive protein (CRP) of 39 mg/L (reference range <1.0 mg/L) and an erythrocyte sedimentation rate (ESR) of 78 mm/h (reference range 0–20 mm/h).
He was taken to the operating room (OR) the following day where 2 areas of pus within the most distal incision and a sinus tract tracking behind the femur and onto the previously placed metal plate were identified.
The area was washed out, the hardware was removed, and he was started empirically on oxacillin.
Aerobic and Anaerobic bacterial cultures were negative except for 2 different isolates of coagulase-negative staphylococcus that were not recovered from plates but grew only from the thioglycolate broth after 4 days suggesting low levels of bacteria.
He was switched from oxacillin to vancomycin 15 mg/kg/dose every 8 hours, resulting in an initial trough level of 6.8 μg/mL.
When his spica cast was removed 5 days postoperatively, a new superficial purulent collection in the middle left lateral femur was noted that required another washout.
He was continued on vancomycin, which had been adjusted to 15 mg/kg/dose every 6 hours, to maintain troughs between 15 and 20 μg/mL, with a maximum trough level of 19.6 μg/mL.
Twenty-two days later, the sutures were removed, and again purulent drainage was found at the lower and mid incision sites of the left lateral thigh
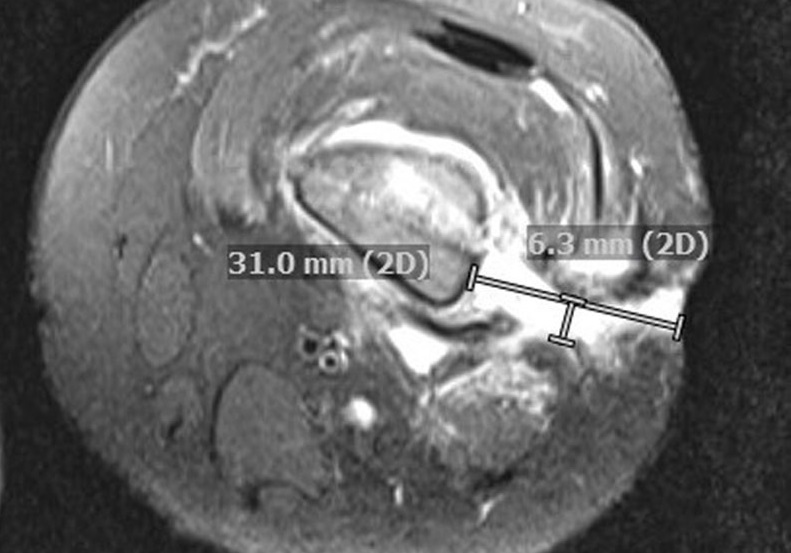
Magnetic resonance imaging (MRI) showed several thin tracts extending from the femur to the skin in addition to diffuse areas of bone marrow, adjacent soft tissue, and muscular edema as well as chronic periosteal reaction (Fig. 1B).
Interestingly, his inflammatory markers had all decreased (CRP 5.3 mg/L, ESR 25 mm/h, and WBC 8.4 × 1000/μL).
Cultures taken during the third incision and drainage in the OR revealed the diagnosis.
One hundred fifty-two days following the initial traumatic MVA, the patient was taken for a third incision and drainage where pus was found at the original incision sites and under the iliotibial band and portions of the vastus lateralis that required debridement.
Several bone biopsies and cultures of purulent fluid from the bone were collected for staining and culture.
Stains were negative for bacterial, fungal, and acid-fast bacilli organisms.
One of 3 cultures of the pus grew 3 colony-forming units of Clostridioides difficile after anaerobic incubation for 3 days.
This was identified by matrix-assisted laser desorption/ionization-time of flight mass spectrometry using the Vitek mass spectrometry (bioMérieux) in vitro diagnostic database.
Bacterial, fungal and acid-fast bacilli cultures of the bone remained sterile, and a molecular test for non-tuberculosis mycobacteria was negative.
Bone biopsies from the distal and mid-left femur showed chronic osteomyelitis.
Repeat MRI 7 days later, revealed an increased non-enhancing region within the distal femoral marrow concerning for necrotic versus purulent material, which communicated with a fluid-enhancing tract toward the skin and a sequestered cortical bone fragment in the mid to distal femur.
Despite continued treatment with IV vancomycin, his inflammatory markers increased: WBC 10.9 × 1000/μL, CRP 42.8 mg/L and ESR 59 mm/h.
Back in the OR, a sinus tract in the distal aspect of the superior incision was debrided, and pus was noted to be tracking down to a subperiosteal abscess.
Empiric metronidazole was started due to the previous positive culture for C. difficile, and vancomycin was continued.
Three of 4 tissue cultures grew C. difficile, after anaerobic incubation. Vancomycin was discontinued following lack of improvement after 6 weeks of therapy.
A follow-up MRI of the left femur 21 days following the last OR intervention re-demonstrated chronic osteomyelitis with persistent draining fistulous tracts but without progression or new findings
His inflammatory markers were: WBC 6.2 × 1000/μL, CRP 0.3 mg/L and ESR 8 mm/h.
He completed 3 weeks of IV metronidazole therapy and was transitioned to oral therapy 188 days following the initial injury.
He remains on oral metronidazole for chronic osteomyelitis.
At his last follow-up visit, his physical examination was significant for no further purulent drainage from the lateral thigh incisions.
He continued to have a mildly elevated ESR of 25 mm/h, but a normal CRP of 0.3 mg/L.
He is planned to undergo sequestrum removal with leg-lengthening.
Persistent_Leg_Drainage_in_a_Pediatric_Trauma.27 drenaggio traumatizzato pediatricoRead Also:
Tourniquet Or No Tourniquet? Two Expert Orthopaedics Speak On The Total Knee Replacement
MEDEVAC In Italy, Main Complications And Treatments In Critical Patients Transport?
Pre-Vac, Portable Sterile Bottle For Closed Wound Drainage
Source:
Howard, Ashley DO*; Rychalsky, Michelle R. PharmD†; Murray, Thomas S. MD, PhD*


