Rapid Blood-Pressure Lowering in Patients with Acute Intracerebral Hemorrhage
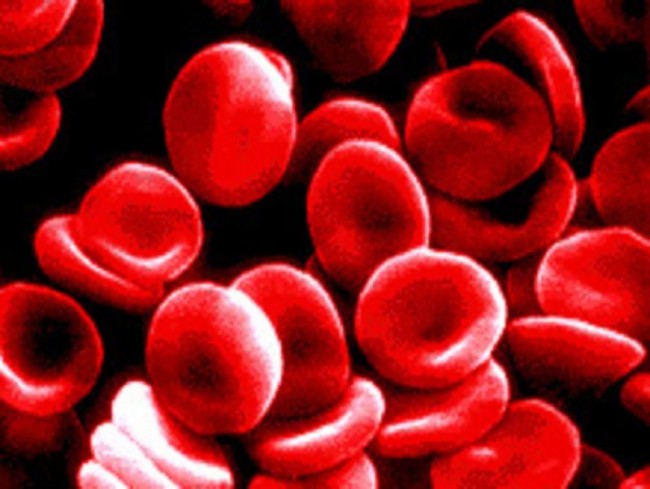
Intracerebral hemorrhage (ICH) is a life-threatening type of stroke that involves bleeding within the brain tissues. Events like hypertension put high pressure on the tiny arteries that supply blood and oxygen to the brain. Too much arterial pressure makes these arteries rupture and eventually blocks blood supply, leading to cell damage.
A stroke like the intercerebral hemorrhage (ICH) arises when the brain doesn’t receive enough blood supply and oxygen, which may be brought by head trauma, hypertension or blood clot formations. This is a medical emergency that requires immediate management which may involve medications, surgery, or simple interventions to reduce blood pressure; however, the effect of blood pressure-lowering to intercerebral hemorrhage is not fully known.
The study on the Intercerebral Hemorrhage (ICH)
The study of Anderson, C. et. al. (2013) assessed the efficiency of intervening Intercerebral Hemorrhage (ICH) through a rapid lowering of blood pressure where it involved the participants’ demographic and clinical features. On the other hand, the sternness of their stroke was assessed through Glasgow Coma Scale (GCS) and the National Institutes of Health Stroke Scale (NIHSS) recorded baseline, at 24 hours and at 7 days or at the time of their hospital discharge.
During the assessment of baseline data, CT scan of the brain or MRI was done in order to confirm stroke which is in line with the existing standard technique. Further, at 28 days or 90 days, the patients were followed-up either by telephone or in-person by a trained local staff unaware of the group assignments. Those patients who were unable to receive the supposed treatment or were unable to adhere with the guidelines were followed up in full, as well as their information was incorporated in the investigation according to the ‘intention to treat’ principle.
What has been verified during the study on the Intercerebral Hemorrhage (ICH)
In the study, the researchers had randomly assigned 2839 patients who had a history of spontaneous intracerebral hemorrhage within the previous 6 hours and who had elevated systolic blood pressure. They were preferred to receive intensive treatment to lower their blood pressure with the goal of lowering the systolic level of <140 mmHg within 1 hour or a guideline-recommended treatment with a goal of the systolic level of <180 mmHg.
The primary outcome was death or major disability, which was described as a score of 3 to 6 on the modified Rankin scale (a score of 0 indicates no symptoms, a score of 5 indicates severe disability, and a score of 6 indicates death) at 90 days. A pre-specified ordinal analysis of the modified Rankin score was also performed as well as the rate of severe adverse events was compared between the two groups. Among the 2794 participants for whom the primary outcome could be determined, 719 of 1382 participants (52.0%) receiving intensive treatment, as compared with 785 of 1412 (55.6%) receiving guideline-recommended treatment, had a primary outcome event.).
Mortality was 11.9% in the group receiving intensive treatment and 12.0% in the group receiving guideline-recommended treatment. Non-fatal serious adverse events occurred in 23.3% and 23.6% of the patients in the two groups, respectively.
In conclusion, in patients with intracerebral hemorrhage, intensive lowering of blood pressure is not effective to significantly reduce the rate of the primary outcome of death or severe disability. However, an ordinal analysis of modified Rankin scores indicated improved functional outcomes with an intensive lowering of blood pressure.
CONTINUE TO READ THE STUDY OF:
Craig S. Anderson, M.D., Ph.D., Emma Heeley, Ph.D., Yining Huang, M.D., Jiguang Wang, M.D., Christian Stapf, M.D., Candice Delcourt, M.D., Richard Lindley, M.D., Thompson Robinson, M.D., Pablo Lavados, M.D., M.P.H., Bruce Neal, M.D., Ph.D., Jun Hata, M.D., Ph.D., Hisatomi Arima, M.D., Ph.D., et al., for the INTERACT2 Investigator
READ ALSO:
Blood Pressure: New Scientific Statement for the Evaluation in People
Will lower blood pressure reduce the risk of heart and kidney diseases or stroke?
Cincinnati Prehospital Stroke Scale. Its role in Emergency Department
Higher risk of stroke for veterans with mental health disorders
Stroke is a problem for people with long work hours shift
Australian first Stroke Ambulance – New frontier for saving lives



