Deep vein thrombosis: causes, symptoms and treatment
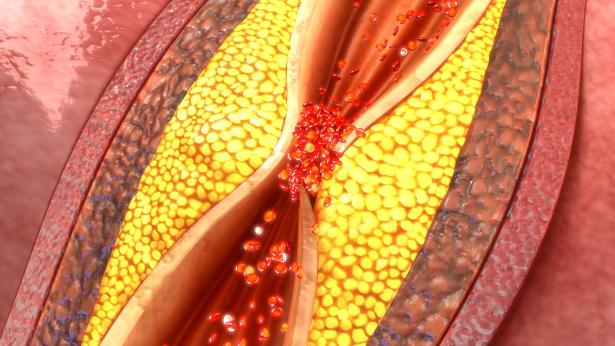
What is deep vein thrombosis? Thrombosis is a pathological process that occurs due to pathological coagulation resulting in the formation of a thrombus that reduces or completely occludes the lumen of a vessel
The most common sites of thrombus formation are the deep veins of the legs and those of the pelvis, but thrombosis can occur in any vein, including the hepatic vein (Budd-Chiari syndrome), renal veins, retinal veins and even the superior and inferior vena cava.
DVT is a disease that is as common as it is often silent.
The incidence in the general population is not decreasing, despite the increasing use of prophylaxis, in connection with the increase in the number of surgeries even in elderly people and the lengthening of life expectancy, with an increasing number of elderly patients bedridden due to chronic diseases.
This high incidence, in the face of prevention and adequate therapies, is due to the increased thrombotic risk in our era due to sedentary habits, use of oestrogen contraceptive therapies, increased incidence of major orthopaedic surgery, and increased incidence and length of cancer diseases with which DVT is often associated.
Signs and symptoms of deep vein thrombosis
Deep vein thrombosis in the leg is sometimes asymptomatic when it is confined to the veins of the calf; in other cases, patients may report tightness or pain in the calf, especially when walking.
If the thrombosis extends to the popliteal vein, the increase in calf volume is more pronounced and may be accompanied by inflammation i.e. heat and reddened skin at the posterior aspect of the calf and turgor of the superficial veins.
If the affected venous tract is above the knee there is a considerable increase in volume of the calf with pain, the oedema may also go up to the thigh depending on the level of obstruction.
The compression of muscle masses is painful, there is a rise in temperature and an increase in heart rate.
In view of the above, it is essential to always suspect DVT and to look for its presence a priori in cases of pulmonary embolism, post-phlebitis syndrome, hip or small pelvis surgery, and in the pre-operative phase of a varicose vein removal operation.
The best clinical sign is the suspicion of DVT on a predisposing ground; in fact, DVT is more frequent in elderly subjects with excess weight, bedridden or with immobilisation of the lower limbs, recent surgery, trauma, venous circulatory disorders, heart failure without antithrombotic prophylaxis.
Certain anamnestic elements of the patient reinforce the suspicion such as the use of estro-progestin birth control pills, family history of DVT, tumours.
Deep vein thrombosis of the leg:
- oedema of the ankle and leg;
- cyanotic (bluish) and warm skin on the affected limb;
- hardened and painful muscles (Bauer’s sign);
- painful percussion of the tibia with the finger (Liscker’s sign);
- coughing and sneezing causing increased venous pressure give pain in the calf and ankle (Louvel’s sign);
- when lying down, the turgidity of the veins on the inner side of the leg is appreciated: the Great saphenous vein dilates due to haemodynamic compensation (Pratt’s sign).
Thrombosis of the femoral and iliac veins:
- fever but not always;
- increased heart rate but not always;
- feeling of heaviness in the affected limb;
- pain in the thigh;
- swollen limb.
Causes and risk factors for deep vein thrombosis
Familiarity: most case histories show an increased risk in individuals with a positive family history of DVT or pulmonary embolism; this may also be due to the fact that certain congenital coagulation alterations, collectively referred to as thrombophilic conditions, such as antithrombin III, protein C or protein S deficiency, Factor V Lieden, Factor II, etc. (there are many known factors to date) are inherited.
Gender: women are generally more affected as a sex due to the venous alterations of pregnancy, possible use of oral contraceptives, more frequent obesity and greater longevity than men.
Age: DVT is rare under the age of 40, except in cases related to pregnancy and puerperium and to thrombophilic conditions; however, after the age of 40 their frequency increases progressively, due to physiopathological changes in the venous wall, with exhaustion of the muscular tonaca, dilation and tortuosity of the superficial veins, and loss of efficiency of the musculovenous pump, i.e. the greater incidence of chronic venous insufficiency in women;
Blood group: DVT is more frequent in subjects with blood group A and rarer in subjects with blood group 0. This may be due to the fact that subjects of blood group 0 have lower levels of factor VIII, whereas in subjects of blood group A, a reduced plasma concentration of antithrombin III, a physiological inhibitor of coagulation, has been advanced.
Body mass: obesity is indicated as a risk factor for DVT as it limits physical activity and delays mobilisation of patients after surgery. In addition, obese subjects often present alterations in lipid metabolism and in particular hypertriglyceridemia, which in turn correlates with inhibition of plasma fibrinolytic activity.
Stasis: the correlation between DVT and prolonged immobilisation due to the slowing of venous return, with consequent stasis, especially in the lower limb district, is widely known. In the literature, cases of DVT have been described in predisposed individuals who have been behind the wheel of a car or in front of the television for a long time. The risk of DVT increases when immobilisation is associated with advanced age.
Nutritional factors: Numerous observations confirm the importance of blood levels of triglycerides in facilitating DVT and the preventive value of bioflavonoids, resveratrol and many fruits and herbs.
Seasonal variations: some authors have reported an increase in thromboembolic diseases in spring and autumn.
Contraception: the use of oral contraceptives can promote DVT and pulmonary embolism, especially in predisposed individuals; however, the risk associated with the use of oral contraceptives appears to be lower with the use of newer preparations containing reduced dosages of oestrogen.
How deep vein thrombosis is diagnosed
Deep vein thrombosis is as common as it is silent as it is one of the most difficult cardiac and vascular diagnoses.
In fact, many deep vein thromboses are totally asymptomatic and only become apparent with complications, namely pulmonary embolism and post-phlebitic syndrome.
The diagnosis is confirmed by visualisation of the thrombus using ultrasound or angiographic techniques.
Although non-specific, certain laboratory tests direct the diagnosis and make it possible to follow the course and effectiveness of treatment: haemochrome (platelets), prothrombin time, INR, fibrinogen, D-Dimer.
Deep vein thrombosis therapy
The aim of DVT therapy is to restore patency of the deep venous circulation by removing the thrombus before it has compromised the valvular system, thereby reducing symptoms and above all preventing pulmonary embolism and other complications.
Basically, it is based on two types of treatment
- anticoagulant drugs, to prevent the extension of thrombosis and the formation of floating terminal flaps, which are free and therefore easily detachable, resulting in embolism;
- elastoadhesive bandaging with materials and techniques that realise the low extensibility of the bandage; elastic restraint will play a role in the next phase to avoid post-phlebitic syndrome and chronic venous insufficiency.
Anticoagulant drugs may act by the following mechanisms
- coagulation factor X inhibitors
- factor II, VII inhibitors
Caval filtering, on the other hand, is a technique that consists of proposing a filter to the vena cava in very selected cases or when anticoagulant treatment is contraindicated or when, despite pharmacological treatment, the DVT is recurrent or when floating clot flaps threatening to detach are demonstrable on iconographic investigations.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Raising The Bar For Pediatric Trauma Care: Analysis And Solutions In The US
Pinworms Infestation: How To Treat A Paediatric Patient With Enterobiasis (Oxyuriasis)
Intestinal Infections: How Is Dientamoeba Fragilis Infection Contracted?
Gastrointestinal Disorders Caused By NSAIDs: What They Are, What Problems They Cause
Intestinal Virus: What To Eat And How To Treat Gastroenteritis
What Is Proctalgia Fugax? Symptoms, Causes And Treatment
Internal And External Haemorrhoids: Causes, Symptoms And Remedies
Haemorrhoids: The Newest Tests And Treatments To Treat Them
What Is The Difference Between Haemorrhoids And Fissures?
Complications Of Haemorrhoids: Simple And Oedematous External Thrombosis



