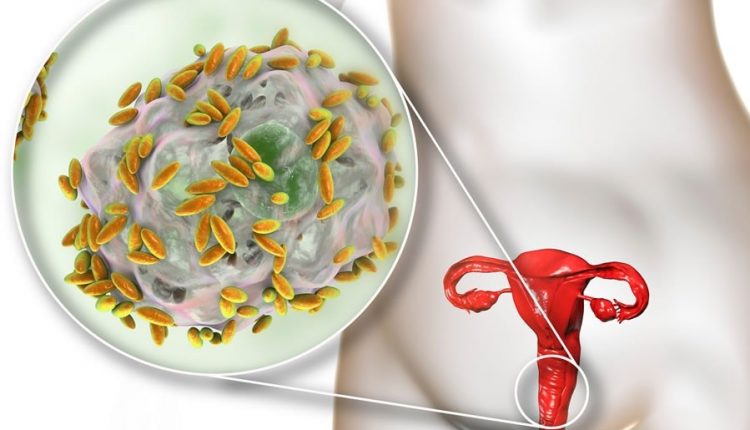
Gardnerella vaginalis vaginosis: symptoms, diagnosis and treatment
Gardnerella is a bacterium, mainly transmitted through sexual intercourse, that causes profuse and foul-smelling vaginal discharge. How is it treated and what are the tips to prevent infection?
What is Gardnerella?
Vaginosis caused by Gardnerella vaginalis is more properly designated as ‘bacterial vaginosis’ as it is an infection in the onset of which several bacteria are involved.
It is characterised by malodorous discharge and vaginal discomfort.
It represents the main infectious disease of the female lower genito-urinary tract: according to recent estimates of the World Health Organisation, it affects up to 40-60% of women of childbearing age (18% in Italy), 15-20% of pregnant women, with a risk of recurrence of 25% at 1 month, 45% at 3 months and 75-80% at 6-9 months.
What causes Gardnerella: the causes
Gardnerella vaginalis is an anaerobic bacterium (which therefore reproduces more easily in poorly oxygenated environments) which, like other anaerobic species such as Mobiluncus and Bacteroides, is present in small quantities in the vaginal bacterial flora of healthy women.
This bacterial flora is predominantly characterised by lactobacilli which, by competition, regulate the physiological balance of the organ and, through the production of lactic acid, defend the genital mucosa from pathogens.
The disruption of the balance between the various components of this vaginal microflora, called the microbiota, leads to an excessive increase in anaerobic bacteria with a concomitant drastic drop in the number, or even disappearance, of lactobacilli.
The decrease in lactobacilli leads to an increase in the vaginal pH, while the excess of anaerobic microorganisms causes an increase in the production of amines (putrescine, cadaverine and trimethylamine) that impart a foul (fish-like) odour to the abundant greyish-white leucorrhoea that covers the vaginal walls.
Risk factors
The vaginal microflora is a dynamic ecosystem, sensitive to exogenous and endogenous influences.
Although Gardnerella vaginitis is not considered a sexually transmitted disease, promiscuous sexual activity and changing partners are risk factors.
Other risk factors, more frequently related to infection, are cigarette smoking, use of IUDs, frequent use of douches.
How to recognise Gardnerella symptoms
Gardnerella vaginalis infection is characterised by abundant greyish leucorrhoea and a fetid (fishy) odour.
The odour is accentuated when vaginal secretions increase: after sexual intercourse, during menstruation and during the ovulatory period.
Many asymptomatic women experience discomfort only in some of these circumstances.
Associated symptoms, which are in fact minimal, include burning during or after sexual intercourse and tension in the lower abdomen.
This dysbiosis can also cause very important complications, such as
- infections in other parts of the genito-urinary system
- obstetrical sequelae such as miscarriages in the 2nd and 3rd trimester, premature rupture of membranes, premature birth, postpartum endometritis, low birth weight of the newborn.
- However, in the majority of cases, it is not a serious infection, although it is very annoying especially because of the strong odour that creates embarrassment and discomfort.
If left untreated, it can persist for months.
Gardnerella in men
The man is to be considered a healthy carrier.
In fact, Gardnerella does not cause discomfort but finds a favourable breeding and storage ground in the smegma, a substance consisting of whitish secretion made up of exfoliated epithelial cells from the mucous membranes, sebum and moist material accumulating under the foreskin.
Only in some cases can the infection result in reddening of the part and disorders of the first urinary tract.
Diagnosis of bacterial vaginosis
Gardnerella vaginosis sometimes resolves spontaneously, especially when asymptomatic; more often, however, it takes on the features of a chronic and recurrent disease.
As the micro-organism is present in small quantities in the vagina of healthy women, its isolation and identification by culture of the bacterium is inadvisable as it would lead to over-treatment.
Malodorous discharge is the most representative symptom of infection, which will be confirmed by other clinical criteria such as
- homogeneous vaginal discharge covering the vaginal walls;
- direct detection of the bacterium by microscopic observation of mucus, smear on a ‘fresh’ slide or treated with special dyes;
- indirect detection by the development of a fishy smell (whiff test) from a slide on which, in addition to the mucus, a few drops of a basic reagent, potassium hydroxide (KOH), are added;
- detection of vaginal pH above 4.5.
How is Gardnerella treated?
Both men and women can be asymptomatic carriers, so treatment with an antibiotic (metronidazole, always prescribed by a doctor) should also be given to the partner.
In the event of resistance to metronidazole, another antibiotic, clindamycin, is suggested.
Both drugs are available for local administration (creams or ova).
In case of antibiotic resistance, chronicity or in pregnancy during which these antibiotics are contraindicated – despite conflicting evidence – treatments with local antiseptics (chlorhexidine, povidone iodide, hydrogen peroxide) and probiotics also seem effective.
Pending a medical examination, if the complaints are bothersome, vaginal douches with a slightly acidic content can be used.
Boric acid, due to its slightly acidic action, is ideal for reducing the pH.
It is found ready-to-use in the form of lavender in a 3% aqueous solution.
Vaginal douches and creams are commercially available, again with a slightly acidic character; the creams should be applied externally, thus leaving the possibility for the doctor to take vaginal samples later, if necessary for diagnostic certainty.
How to prevent bacterial vaginosis
Vaginosis caused by Gardnerella vaginalis is very common in the healthy population.
Moreover, the scarcity of symptoms makes diagnosis difficult and effective prevention problematic.
Useful recommendations are the use of condoms during promiscuous sexual intercourse or in the case of a new partner, and prompt treatment as soon as the disorder is felt.
The use of screening with slides stained with special dyes (Gram) in asymptomatic pregnant women is the subject of controversy; on the other hand, the use of diagnostic screening (i.e., irrespective of symptoms) in the case of pregnant women with a history of unfavourable obstetrical outcomes, such as previous preterm delivery or late abortion, seems worthy of consideration.
When to seek medical advice?
Very often patients suffering from gardnerella vaginalis look for a way to quickly relieve the unpleasant discomfort on their own.
They resort to creams or ova, which not only do not solve the problem but can even delay the correct detection of the bacteria responsible for the disorder and, therefore, the cure.
This is why it is essential not to try to treat bacterial vaginitis on one’s own, relying on over-the-counter remedies or a friend’s advice, but to consult a specialist in order to make an early diagnosis.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Vaginal Yeast (Candidiasis): Causes, Symptoms And Prevention
Chlamydia, Symptoms And Prevention Of A Silent And Dangerous Infection
Vulvodynia: What Are The Symptoms And How To Treat It
What Is Vulvodynia? Symptoms, Diagnosis And Treatment: Talk To The Expert
Accumulation Of Fluid In The Peritoneal Cavity: Possible Causes And Symptoms Of Ascites
Accumulation Of Fluid In The Peritoneal Cavity: Possible Causes And Symptoms Of Ascites
What’s Causing Your Abdominal Pain And How To Treat It
Pelvic Varicocele: What It Is And How To Recognise The Symptoms
Can Endometriosis Cause Infertility?
Transvaginal Ultrasound: How It Works And Why It Is Important
Candida Albicans And Other Forms Of Vaginitis: Symptoms, Causes And Treatment
What Is Vulvovaginitis? Symptoms, Diagnosis And Treatment
Vaginal Infections: What Are The Symptoms?



