Study Finds Link Between Colon Cancer and Antibiotic Use
Colon cancer and antibiotic: traditionally, colorectal cancer was a condition that mostly impacted older people. But it’s now the third leading cause of cancer deaths in young adults
The exact reason has puzzled researchers for years, but a new study suggests a surprising potential link: antibiotic use.1
The study, which was published in the British Journal of Cancer, analyzed primary care data from 1999 to 2011 from nearly 40,000 people.
The researchers specifically looked at antibiotic use and lifestyle factors of people who developed colorectal cancer and those who did not.2
While overall cancer numbers were low (7,903 people developed colon cancer and 445 were under the age of 50), the researchers found that those under 50 who used antibiotics had a 50% higher risk of colon cancer than those who didn’t.
Those who were 50 and over who used antibiotics had a 9% greater risk of developing colon cancer.
The more people used antibiotics, the greater their risk.
What Is Colon Cancer?
Colon cancer is often mentioned in the broader sense of colorectal cancer, which is an umbrella term used to reference cancers of the colon and rectum.
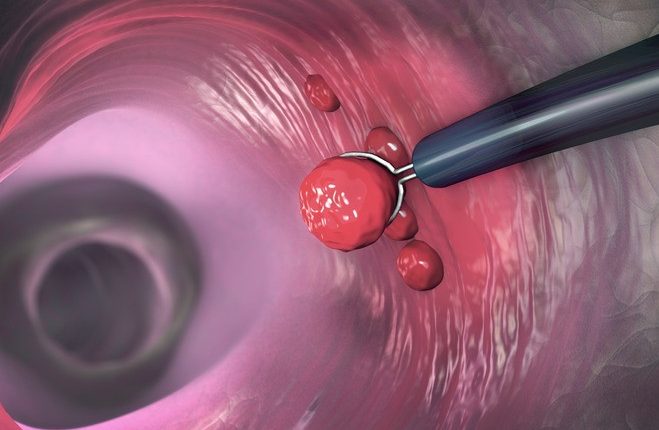
Most colorectal cancers start as a growth called a polyp on the inner lining of the colon or rectum.
These polyps can change into cancer over time.3
Colorectal cancer is the third most common cancer diagnosed in men and women in the U.S.4
There didn’t seem to be a link between antibiotic use and rectal cancer, though.
“Our findings suggest antibiotics may have a role in colon tumor formation across all age groups,” the researchers concluded.
Why Might Antibiotic Use Raise the Risk of Colon Cancer?
The study itself just focused on the association—not the reasons why using antibiotics could increase the risk of colon cancer.
However, there are some theories about why this might be the case.
Scott Kopetz, MD, PhD, a gastrointestinal oncologist at the University of Texas MD Anderson Cancer Center, told that antibiotic use may interfere with bacteria in the gut microbiome, which makes up a world of microorganisms that populate our gastrointestinal tract.
“A healthy microbiome has a mixture of multiple different types of bacteria that can maintain a healthy state for the cells lining the colon wall,” he said.
“The use of antibiotics can disrupt this healthy microbiome and may, over time, result in a higher risk of colorectal cancer.”
Anton Bilchik, MD, PhD, MBA, FACS, a surgical oncologist and director of the gastrointestinal research program at Saint John’s Cancer Institute at Providence Saint John’s Health Center in California, agrees that the gut microbiome may be impacted by antibiotic use.
“The possible explanation for why antibiotics may be associated with an increased risk is not completely clear, but some bacteria in the microbiome work with the immune system to protect against colon cancer,” he told.
Antibiotics may be neutralizing the good bacteria and stimulating the bad bacteria, increasing the chance of colon cancer
Sarah Hoffe, MD, section head of GI radiation oncology at Moffitt Cancer Center, told that the specific findings lend credibility to these theories.
“The highest cancer risk was seen in patients taking the most antibiotics but the studies have shown even a small elevated risk after a single course of antibiotics,” she said.
“The increased risk was seen primarily in the right side of the colon known as the proximal or ascending colon where there is higher bacterial activity than other parts of the intestine.”
What This Means For You
Antibiotic use is linked to an increased risk of colon cancer in younger people
. While there isn’t a direct cause and effect established, experts recommend only using antibiotics when you need them, just to be safe.
How to Approach Antibiotic Use
Experts stress that people shouldn’t avoid using antibiotics when they need them for fear of developing colon cancer.
There is just a link at this point—not a proven cause—and plenty of people use antibiotics with no issues.
“Antibiotic use is so common that confounding factors may be contributory to the increased risk of colon cancer,” Hoffe said.
Kopetz said there can also be less obvious associations that can explain the link.
“Patients who are more likely to see a doctor on a regular basis, for example, would be more likely to receive antibiotics and may also be more likely to undergo colonoscopy screening for cancer detection,” he said.
Still, Bilchik said that the findings are credible.
“If you need antibiotics, you should take them. But clearly, antibiotics are overprescribed,” he said.
“This is just another reason why the judicious use of antibiotics is important.”
Overall, Kopetz recommends that people do their best to eat a healthy diet and exercise regularly to lower their risk of colon cancer, along with getting screened.
“Obtaining the recommended screening starting at the age of 45 can result in early detection of cancer and prevention through removal of precancerous lesions,” he said.
References:
- American Cancer Society. Key Statistics for Colorectal Cancer.
- McDowell R, Perrott S, Murchie P, Cardwell C, Hughes C, Samuel L. Oral antibiotic use and early-onset colorectal cancer: findings from a case-control study using a national clinical database. Br J Cancer. 2021. doi:10.1038/s41416-021-01665-7
- American Cancer Society. What Is Colorectal Cancer?
- American Cancer Society. How Common Is Colorectal Cancer?
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Ulcerative Colitis: What Are The Typical Symptoms Of The Intestinal Disease?
Wales’ Bowel Surgery Death Rate ‘Higher Than Expected’
Irritable Bowel Syndrome (IBS): A Benign Condition To Keep Under Control
Intestinal Infections: How Is Dientamoeba Fragilis Infection Contracted?




