Urinary tract infections: symptoms and diagnosis of cystitis
Let’s talk about cystitis: urinary tract infections are a major health problem due to their prevalence and morbidity
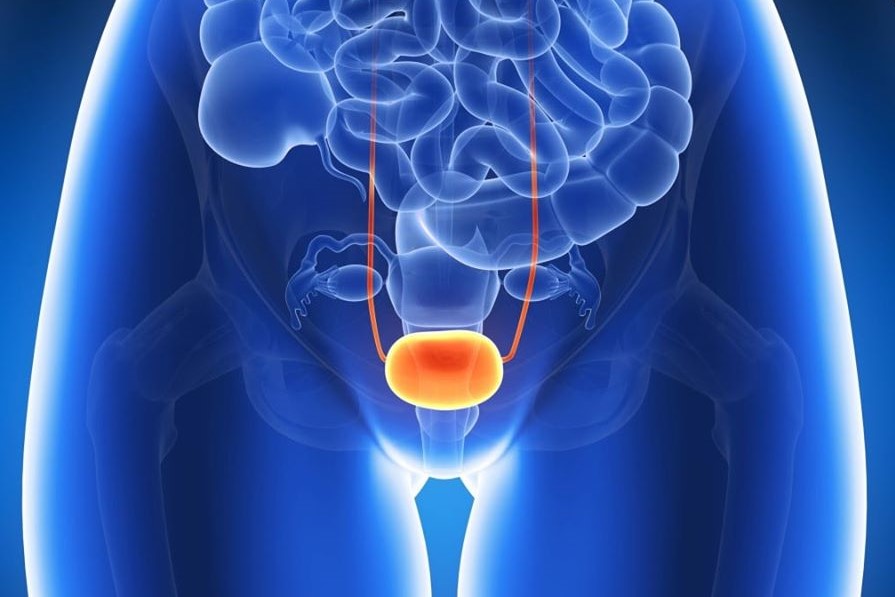
They represent an inflammatory process of an infectious nature affecting a part of the lower urinary tract, the bladder, characterised by the presence of a significant bacterial load.
In the United States, they are responsible for approximately seven million outpatient visits and more than one million hospital admissions each year.
In 1863, the great Luis Pasteur demonstrated that urine can allow bacterial growth. The growth and subsequent development of bacteria can occur in the kidneys (pyelonephritis), in the bladder (cystitis), in the urethra (urethritis), and in the prostate (prostatitis).
Cystitis is nothing more than an inflammation of the urinary bladder
It is caused by an ascending infection and can vary from a simple phlogistic process to a serious pathology that can sometimes migrate to affect the upper urinary tract, i.e. the kidneys, leading to death by uremia.
Fortunately, this scenario occurs very rarely.
In addition to occurring due to an ascending infection, it may develop from a renal infection, such as tuberculosis, schistosomiasis or other primary kidney infections.
In adult women, this pathology, especially when limited to the trigone, is mainly due to ascending urethritis.
In children, girls and adult men, the presence of recurrent episodes of cystitis indicates a physiological or anatomical abnormality for which the pathology must be investigated by means of specific diagnostic tests.
The inflammatory process of the bladder mucosa can vary greatly in degree and this depends on both the virulence of the infecting agent and the resistance of the host.
Acute bacterial cystitis is a common disease in females
Approximately 25 – 30 % of women between 20 and 50 years of age report a history of urinary tract infection on examination.
People who have had an acute episode of cystitis are familiar with the painful symptoms and, above all, the consequences that such symptoms can have on their daily life and sex life.
We cannot consider it as a single disease but as a group of diseases.
In fact, on the one hand we find women with isolated or infrequent infections, and on the other, women with recurrent and intolerably recurrent infections.
This pathology can also cause serious infectious complications at the kidney level and not inconsiderable problems at the bladder level or present coexistence with Candida Albicans, which arises after antibiotic therapy as a demonstration of a drop in immune defences and metabolic alterations.
Chronic bladder infections can also be predisposing causes for bladder cancer, today the fourth leading cause of death worldwide.
Cystitis can be of various types:
- bullous or polypoid cystitis: characterised by the presence of inflammatory oedema that raises the bladder mucosa, a pathological condition that could affect an infection of adjacent organs;
- ulcerative and haemorrhagic cystitis: both represent a pathological condition of massive infection;
- glandular cystitis: vesicles with a clear or cloudy liquid content cover the bladder wall;
- cystic cystitis: when the above-mentioned vesicles are large in size. In this case both ureters and kidneys may be affected by the pathology.
- chronic interstitial cystitis or Hummer’s ulcer: represented by a chronic inflammation of all layers of the bladder wall. This type of cystitis develops more in the female sex and if not treated correctly and in a timely manner can lead to a severe and progressive decrease in bladder capacity.
The onset of cystitis is greater in girls and women because of their anatomical conformity: a much shorter urethra than in men and its proximity to the anal orifice.
In fact, the infection normally ascends from the urethra into the bladder.
Initial bacteriuria results mainly and usually from the ascending faecal flora along the urethra into the bladder.
In women, colonisation of the mucosa of the vaginal vestibule is a key step in the pathogenesis of urinary infections.
This pattern of ascending lower urinary tract infection is favoured by:
- predisposing factors unintentional introduction of faecal material into the urethral meatus (faecal contamination of the perineum);
- by incomplete bladder emptying, urinary stasis (sclerosis of the bladder neck – cystocele – bladder prolapse – cervical-trigonitis – neurological bladder
Prostatic hypertrophy, in men:
by iatrogenic means that exceed functional lines of defence against germs (intermittent or permanent catheterisation).
Cystitis, however, can also affect the upper urinary tract (kidneys), causing pyelonephritis, caused by
- by functional alterations of the uretero-vesical junction, due to developmental disorders (vesicoureteral reflux);
- by transient vesicoureteral reflux associated with tissue oedema from bacterial cystitis.
The other routes of invasion of the parenchyma, lymphatic and haematogenous, are not common in normal subjects: in fact, lymphatic dissemination may occur only in cases of major intestinal infections, while haematogenous dissemination may occur in patients with bacteremia caused by Staf. Aureus or Candida fungemia.
Urinary infections, predisposing to bacterial cystitis, can be divided into 4 categories :
- Isolated infections occur in 30 to 40% of women, between 27 and 42 years of age. They represent the first episode of urinary infection or infections that recur after an interval of at least 6 months;
- unresolved infectionswhen drug treatment has failed to sterilise the urine;
- re-infections are those that account for 90% of recurrent urinary infections;
- persistent infections when there is a recurrence of the urinary infection, caused by the same infecting micro-organism, starting from an outbreak within the urinary tract.
This disease is also very common in pregnant women and the elderly.
Symptomatology of cystitis
The clinical picture manifests itself with irritative symptoms such as:
- malaise
- suprapubic or lower intestinal pain;
- pain during the sexual act, resulting in decreased sexual desire;
- nocturia;
- imperative urination;
- burning urination;
- dysuria, desire to empty the bladder often, even if urination is painful and low in quantity;
- urine often slightly darker; presence of microhaematuria (blood in urine);
- often foul-smelling urine.
Bacterial cystitis in young women is caused by aetiological agents, with predictable antimicrobial susceptibility profiles
Escherichia coli (80%);
Saprophyticus (5 – 15 %);
Klebsiella (10 – 15 %);
Proteus Mirabilis and other intestinal microorganisms.
As can be seen, the bacterium most responsible for baptismal cystitis is Escherichia coli, called the ‘super-mutant’.
It appears to have a great capacity to survive in the human body and to rapidly mutate in such a way that it can resist antibiotic treatment for a period of time.
Escherichia coli can survive in an acidic environment, multiplies at great speed and adapts to any environment.
As one of the most dangerous pathogens to live with, it is coated and covered with micro-cilia consisting of lectins that bind to the mannose present on the bladder and urinary tract mucosa.
Diagnosis of cystitis
The urologist, after collecting an accurate remote and proximate family history of the patient or patient’s pathology, should subject him or her to a thorough medical examination to assess the presence of current pathology, the possibility of the presence of a cystocele or bladder prolapse (in women) or prostatic hypertrophy and sclerosis of the bladder neck (in men).
- Laboratory and diagnostic tests to be performed
- the blood count may show a modest leukocytosis;
- urine examination with urinoculture and antibiogram; the pathogenic germs responsible for the infection in progress will be identified, which can be eradicated with appropriate and targeted sntibiotic therapy;
- Bladder ultrasonography with evaluation of residual post urination to exclude the presence of bladder neck sclerosis, stress bladder, cystocele, bladder prolapse and other bladder pathologies;
- micturition urethrocystography (in order to assess post-minctional residual, bladder neck sclerosis, urethral stenosis);
Control urethrocystoscopy, when episodes of cystitis occur periodically throughout the year (possible interstitial cystitis).
There are two types of therapy, which must not be confused, suppressive and sarmacological
Suppressive, refers to and is implemented when faced with a persistent focus of infection. For example, a patient with bladder or kidney stone lithiasis, with episodes of persistent recurrent infections, after targeted antimicrobial prophylaxis, will have the pathogen removed.
Antimicrobial prophylaxis is implemented in patients, who have recurrent episodes of urinary infections and cystitis. The biological basis of antimicrobial prophylaxis is the eradication of pathogenic bacteria from the anatomical reservoirs (vaginal vestibule – faeces) and there should be no bacterial resistance.
It is mainly based, after urine examination with Urinoc and ABG, on the administration of cycles of specific antibiotics in small doses and is administered, before going to bed, for a continuous period of 3 months, after which it can be discontinued.
If infections develop during this period, they must be treated with the same drug, but in a therapeutic dosage and for about 10 to 14 days, after which the prophylaxis cycle must be resumed, also taking milk enzymes and multivitamin supplements.
With the use of bacterial prophylaxis, studies have shown that there is a considerable reduction in the re-infection rate, from 2 – 3 per patient-year, to 0.1 – 0.4 per patient-year.
If sexual intercourse has a temporal correlation with urinary tract infections, post-coital antimicrobial therapy should be performed with agents such as Nitrofurantoin, Sulfamethoxazole-Trimethoprin and Ciprofloxacin, Levofloxacin, pharmacological molecules that reduce the rate of reinfection.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Cystitis, Antibiotics Are Not Always Necessary: We Discover Non-Antibiotic Prophylaxis
Polycystic Ovary Syndrome: Signs, Symptoms And Treatment
Vulvodynia: What Are The Symptoms And How To Treat It
What Is Vulvodynia? Symptoms, Diagnosis And Treatment: Talk To The Expert
Accumulation Of Fluid In The Peritoneal Cavity: Possible Causes And Symptoms Of Ascites
What’s Causing Your Abdominal Pain And How To Treat It
Pelvic Varicocele: What It Is And How To Recognise The Symptoms
Can Endometriosis Cause Infertility?
Transvaginal Ultrasound: How It Works And Why It Is Important
Candida Albicans And Other Forms Of Vaginitis: Symptoms, Causes And Treatment
What Is Vulvovaginitis? Symptoms, Diagnosis And Treatment


