Corneal keratoconus, corneal cross-linking UVA treatment
Keratoconus is a rare disease affecting the cornea. Surgery is used to stop or delay the development of the disease. The use of vitamin B2 eye drops is essential
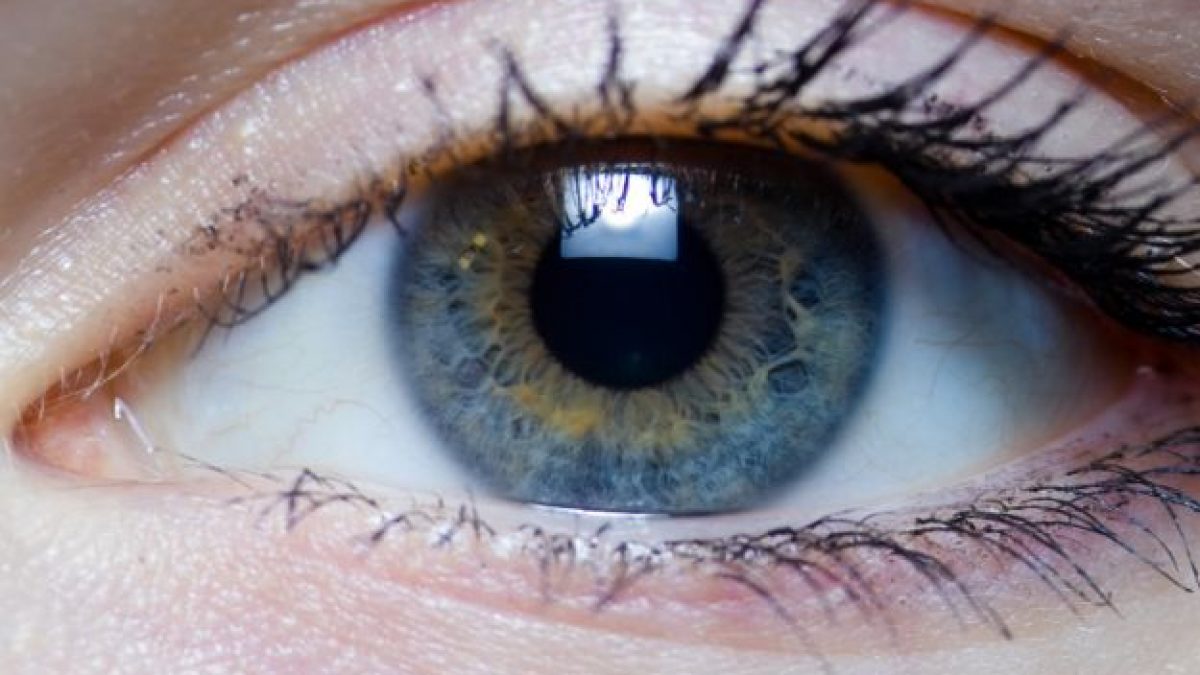
The cornea is the outer lens of the eye
It is the first lens that light rays encounter on their way to the retina where they will form the images that will then reach the brain via the optic nerves.
It is necessary for the light rays to reach the retina in focus.
The cornea is responsible for about 80 per cent of the focusing, the rest is completed by the crystalline lens, which is the inner lens of the eye.
In order to have perfectly focused images on the retina, the cornea must have a regular shape, spherical in the centre and slightly flatter in the periphery.
Certain diseases, such as congenital corneal opacities, eye trauma involving the cornea and corneal infections, lead to a progressive alteration of the shape of the cornea and its thinning.
They thus cause a reduction in visual acuity that is all the more severe the more deformed the cornea is.
The most frequent of these diseases is ‘keratoconus’
In the early stages, the patient is able to compensate for the defect with glasses; as the keratoconus worsens, glasses will no longer suffice and it will be necessary to resort to contact lenses and then, in advanced stages, to surgery.
All surgical procedures, however, are not without their drawbacks due to the unpredictability of scarring reactions of the cornea and, in the case of corneal transplantation, the risk of rejection, which can weaken or opacify it.
This complication is, however, quite rare.
Corneal diseases, what is keratoconus?
It is a progressive disease of the cornea with a hereditary character, characterised by a progressive deformation of the cornea, which tends to take the shape of a cone and become thinner.
Keratoconus occurs most often at puberty and progresses during adolescence to the second and third decade of life.
It has a variable evolution and at the beginning causes progressive astigmatism, worsening vision.
When it appears early, in childhood, it tends to have a more rapid and aggressive course.
In more advanced stages, the cornea thins and stretches outwards.
To date, there has never been a proper therapy for keratoconus
Attempts have been made to reduce its impact on vision by correcting the astigmatism caused by the disease, first with glasses and then with contact lenses.
In the more advanced stages of the disease, the deformation of the cornea is such that it cannot be corrected with either glasses or contact lenses.
In addition, the cornea can become thinner and stretch outwards, becoming opaque, or so ‘fragile’ that it can become perforated.
In these cases, the only therapy remains surgery, which, depending on the stage and speed of evolution of the disease, may consist of:
- In photoablation with an excimer laser;
- In the implantation of plastic ring segments in the thickness of the cornea;
- In lamellar corneal transplantation (i.e. of a layer of the cornea);
- In perforating transplantation (i.e. full-thickness transplantation).
In recent years, a genuine keratoconus treatment has been developed based on a method that ‘strengthens’ the structure of the keratoconus-affected cornea by consolidating the bonds between the corneal collagen fibres.
Human studies show that this treatment is able to slow down the development of keratoconus.
This method of keratoconus treatment aims to halt or delay the evolution of the ongoing process.
If rigidly structured contact lenses are being used, it will be necessary to discontinue them for an appropriate period to be determined by the ophthalmologist.
The method of ‘corneal reinforcement by collagen interlinking’, known as ‘cross-linking’, involves the instillation of an eye drop containing vitamin B2, or riboflavin, which must penetrate the middle layers of the cornea.
In order for riboflavin to penetrate, mechanical removal of the corneal epithelium is required after instilling a few drops of local anaesthetic eye drops.
However, there are also methods that are performed without removal of the corneal epithelium.
In uncooperative patients and children it can be performed under general anaesthesia.
After removal of the corneal epithelium and the application of riboflavin in eye drops, the cornea is subjected to a low-dose irradiation with ultraviolet type A (UVA) radiation, which lasts 30 minutes.
During UVA irradiation, riboflavin application is repeated every 5 minutes
At the end of UVA exposure, the eye is medicated with eye drops or antibiotic ointments and closed with bandages or a therapeutic contact lens for about 3-4 days.
The bandage or contact lens applied at the end of the treatment serves to allow the reformation of the corneal epithelium removed during the operation.
Until the corneal epithelium has fully reformed, vision may be blurred and pain or foreign body sensation may occur, which can be controlled by taking painkillers by mouth.
Visual improvement after treatment begins to be perceptible after complete re-epithelialisation of the cornea and must be verified after a careful “vision measurement” (complete refractive examination).
Studies have shown that this treatment produces no side effects on other parts of the eye (corneal endothelium, crystalline lens, retina) and does not lead to scar formation.
The most frequently encountered side effect is temporary oedema of the cornea, which normally disappears with complete re-epithelialisation.
The process of corneal re-epithelialisation may occur more slowly than usual, depending on individual biological variability, which cannot be predicted.
In this case, painful symptoms, foreign body sensation and a certain degree of corneal oedema may be present for longer than the usual 3-4 days and require regular administration of local antibiotic therapy and oral painkillers.
However, more severe cases of persistent corneal opacification following treatment have been described.
Thanks to the action of riboflavin, irradiation with UVA rays leads to the interlacing and strengthening of the corneal collagen.
This reinforcement consolidates and makes the cornea more resistant to the wear and tear that characterises keratoconus
In a number of cases, in addition to slowing down the wear and tear, this treatment has been shown to reduce astigmatism by improving natural vision.
At the end of the postoperative period it may be necessary to re-evaluate the optical correction with both glasses and contact lenses.
Contact lens wear can only be resumed on the prescription of the ophthalmologist.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Myopia: What It Is And How To Treat It
Presbyopia: What Are The Symptoms And How To Correct It
Nearsightedness: What It Myopia And How To Correct It
Blepharoptosis: Getting To Know Eyelid Drooping
Lazy Eye: How To Recognise And Treat Amblyopia?
What Is Presbyopia And When Does It Occur?
Presbyopia: An Age-Related Visual Disorder
Blepharoptosis: Getting To Know Eyelid Drooping
Lazy Eye: How To Recognise And Treat Amblyopia?
What Is Presbyopia And When Does It Occur?
Red Eyes: What Can Be The Causes Of Conjunctival Hyperemia?
Autoimmune Diseases: The Sand In The Eyes Of Sjögren’s Syndrome
Corneal Abrasions And Foreign Bodies In The Eye: What To Do? Diagnosis And Treatment
Covid, A ‘Mask’ For The Eyes Thanks To Ozone Gel: An Ophthalmic Gel Under Study
Dry Eyes In Winter: What Causes Dry Eye In This Season?
What Is Aberrometry? Discovering The Aberrations Of The Eye
Dry Eye Syndrome: Symptoms, Causes And Remedies


