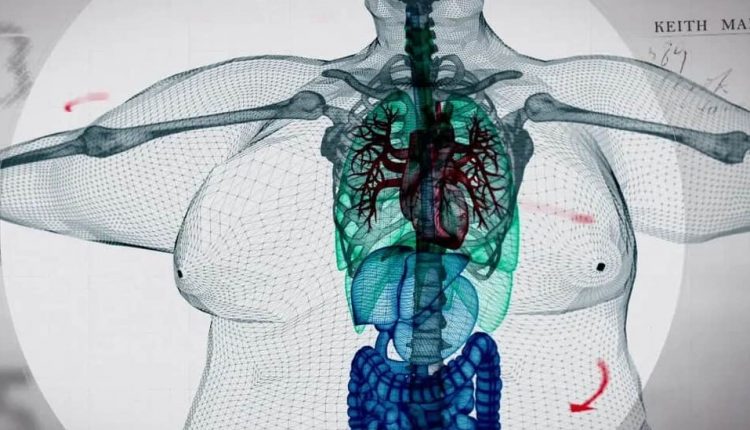
Obesity: what is bariatric surgery and when to do it
With regard to obesity, when we talk about bariatric surgery we mean a set of interventions that are essential for obese people, both to eliminate excess fatty tissue and to prevent or treat the pathologies associated with obesity
If, in fact, various therapies are possible to combat an overweight situation, when one has to deal with major obesity, of 2nd or 3rd degree, the only solution is bariatric surgery.
Obesity is a pathology caused by an increase in adipose tissue, which shortens life expectancy and worsens the quality of life, as it is associated with various diseases, metabolic (type 2 diabetes, high cholesterol and triglycerides), cancer, and cardiovascular and respiratory diseases.
Bariatric surgery: the operations
Bariatric surgery encompasses all those surgical procedures aimed at weight reduction in those suffering from obesity, and the treatment of associated diseases.
These are minimally invasive operations, which are performed laparoscopically: laparoscopy, combined with modern and effective management of the perioperative period, allows the patient to benefit from a faster recovery, a short hospital stay and reduced post-operative pain.
Following bariatric surgery, the patient must follow a long follow-up course to ensure the success of the surgery through weight maintenance and reduction of possible side effects of bariatric procedures.
On average, bariatric surgery results in a weight loss of 70% of the excess kilos, but the loss may vary depending on the age, height, gender and medical history of the patient.
Gastric bypass and sleeve gastrectomy: what are the differences?
There are four internationally validated bariatric procedures, but two alone (Sleeve Gastrectomy and Gastric Bypass) account for more than 80% of the procedures performed worldwide.
Then there are other procedures that were more easily performed in the past but are now almost in disuse, such as gastric banding and biliopancreatic diversion.
Sleeve gastrectomy involves a vertical resection of a significant part of the stomach.
It reduces the sense of hunger and increases the feeling of satiety, so operated persons lose weight because they eat little, but do so spontaneously, without effort.
In the long term, it is a very well-tolerated procedure.
Gastric bypass surgery has been practised for more than 50 years now.
Here too, weight is lost through reduced hunger and increased satiety, but there is also a component of reduced intestinal absorption.
Gastric bypass is particularly indicated in cases of advanced type 2 diabetes and in cases of severe gastro-oesophageal reflux.
As for the now less common interventions, gastric banding involves placing a silicone ring around the upper part of the stomach.
It is a lower-risk operation, but its low efficacy, together with the high rate of second operations (due to failure or side effects) make it little appreciated by both patients and surgeons.
Biliopancreatic diversion, on the other hand, is a particularly effective but also complex operation with a high risk of side effects.
This is why, although it has been practised since 1976, it is only reserved for very special cases, carefully assessed by the specialist.
Cardiovascular disease, respiratory insufficiency and cancer: the consequences of obesity and the role of bariatric surgery
The aim of bariatric surgery is twofold: weight loss and resolution or prevention of the serious, even fatal, long-term comorbidities that obesity entails.
A longitudinal study, carried out at the University of Utah, confirmed what has already been seen in previous studies.
In 40 years of observation of 45,000 subjects suffering from obesity (half treated with surgery and half treated with non-surgical therapies), the mortality rate of the operated subjects was 72% lower for diabetes, 43% lower for cancer and 29% lower for major cardiovascular events.
There are now numerous international studies showing a 50% decrease in mortality in obesity patients who underwent bariatric surgery compared to obesity patients who did not undergo surgery.
Obesity can lead to the onset of diseases such as:
- type 2 diabetes mellitus
- high blood pressure
- increased blood cholesterol and triglycerides
- sleep apnoea.
These disorders, either individually or combined and reinforcing each other, can cause heart attack, stroke and pulmonary embolism.
Obesity is also a risk factor for respiratory failure, osteoarthritis and cancers such as those of the breast, uterus, colon, pancreas and liver.
Bariatric surgery: when to have the operation?
Bariatric surgery is a suitable option for all persons aged between 18 and 65 years, suffering from second-degree obesity (body mass index or BMI equal to or greater than 35) with associated diseases, such as type 2 diabetes, high blood pressure, sleep apnoea, dyslipidaemia, osteoarthritis or previous cardiovascular events, or third-degree obesity (body mass index or BMI equal to or greater than 40) without associated diseases.
For those who have doubts about their body mass index, this is calculated by dividing the weight in kilos by the height in metres squared: to give an example, a person who weighs 120 kg and is 1.7 m tall will have a BMI of 41.5 (120 / 1.702). But if in doubt, automatic BMI calculators can easily be found on the Internet.
There are also contraindications: bariatric surgery cannot be applied in the absence of previous conservative attempts (diet followed by a specialist), and in case of inability to cooperate in the follow-up for the best success of the operation: bariatric surgery is therefore not recommended for those suffering from alcoholism, drug addiction, bulimia nervosa or decompensated psychosis.
Obesity: how to prevent it
Overweight patients must take special care to prevent obesity by implementing a number of health strategies and rules. First and foremost, it is essential that those with excess weight change their lifestyle, making sure they exercise regularly and eat a healthy, balanced diet.
Today, there are injection drugs (liraglutide, semaglutide and, in the future, tirzepatide), initially created for diabetes therapy but which have a powerful anti-hunger effect, which are able to make one lose 10 to 20 kilos of weight without causing hypoglycaemia (as insulin and other anti-diabetic drugs can do). Their use can be of great help in overweight individuals in preventing obesity: of course, the prescription of these drugs must be within a diet.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Obesity And Bariatric Surgery: What You Need To Know
Eating Disorders: The Correlation Between Stress And Obesity
Mindful Eating: The Importance Of A Conscious Diet
In Search Of A Personalised Diet
The Diabetic Diet: 3 False Myths To Dispel
Why Is Everyone Talking About Intuitive Eating Lately?
Climate Change: The Environmental Impact Of Christmas, How Significant It Is And How To Reduce It
Holidays Over: The Vademecum For Healthy Eating And Better Fitness
Mediterranean Diet: Getting Back In Shape Relies On Anti-Ageing Foods
Bloated Belly: What To Eat During The Holidays
Traveller’s Diarrhoea: Tips To Prevent And Treat It
Jet Lag: How To Reduce Symptoms After A Long Journey?
Diabetic Retinopathy: The Importance Of Screening
Diabetic Retinopathy: Prevention And Controls To Avoid Complications
Diagnosis Of Diabetes: Why It Often Arrives Late
Diabetic Microangiopathy: What It Is And How To Treat It
Diabetes: Doing Sport Helps Blood Glucose Control
Type 2 Diabetes: New Drugs For A Personalised Treatment Approach
The Diabetic Diet: 3 False Myths To Dispel
Paediatrics, Diabetic Ketoacidosis: A Recent PECARN Study Sheds New Light On The Condition
Sugars: What Are They Good For And When Are They Bad For Us?
Lifestyle, The Best Ally In Preventing Obesity



