Skin melanoma: types, symptoms, diagnosis and the latest treatments
Melanoma risks: summer is approaching and with it the time for sunbathing, which should always be taken with the necessary precautions
According to multiple studies, the last decade has seen an increase worldwide, particularly in the 30-50 age group, in cases of melanoma, an increasingly common malignant skin cancer.
What is melanoma
Melanoma is a malignant neoplasm that originates from melanocytes, the cells that are responsible for producing melanin, the natural pigment that protects us like a shield from UV rays that can, over time, trigger a series of carcinogenic and ageing processes.
This form of cancer develops
- mainly on the skin;
- more rarely on the mucous membranes (mouth, nose, anus, vulva/vagina etc.) and on extracutaneous areas (eye and inner ear).
The 4 types of melanoma
Four types of melanoma can be distinguished:
- superficial spreading, the most common form that originates in the superficial part of the skin;
- lentigo maligna, rarer and typical of advanced age, usually develops from a sunspot and skin that has been overexposed to the sun;
- acral lentigo acralis, also less common, presents with the appearance of a bruise/lesion and usually originates in peripheral sites (palm of the hand, sole of the foot, nails, genitals, etc.);
- nodular melanoma, the most aggressive form, which accounts for about 10/15% of all diagnosed cases of melanoma and one of the main causes of death from this disease.
While the first three forms are initially characterised by superficial spread, nodular melanoma spreads deeply from the start, with a prognosis that is, therefore, more difficult.
The symptoms for melanoma and the 5 parameters for self-observation
The general parameters to be observed also and above all independently in skin spots have been indicated with the ABCDE guideline scheme, which recalls the first letters of the alphabet.
These are precisely
- asymmetry: a melanoma has an irregular shape, whereas a benign mole has a rounded appearance;
- borders: they are jagged or indefinite, whereas those of benign moles appear sharp;
- colour: melanocytic lesions have an uneven colouring with different and uneven shades. In a small percentage the melanoma is also colourless (achromic amelanotic melanoma);
- diameter: today this is an outdated parameter. Although in the past only nevi above 6 mm in diameter were considered at risk, current early diagnosis allows melanomas to be detected even at a very early stage, i.e. small in size;
- evolution: attention must be paid if the changes inherent in the 4 previous categories occur in a skin spot within a short period of time.
It is necessary to become accustomed to periodically scrutinising the skin even in peripheral areas, using a mirror and another person, and also to pay close attention to moles that cause
- local discomfort, such as itching
- burning for more than 1 week;
- bleeding.
Dermatological examination: Mole mapping
A good practice is to have regular specialist check-ups, at least once a year or more frequently for those at risk, even before puberty, in order to identify patients who may have a greater predisposition.
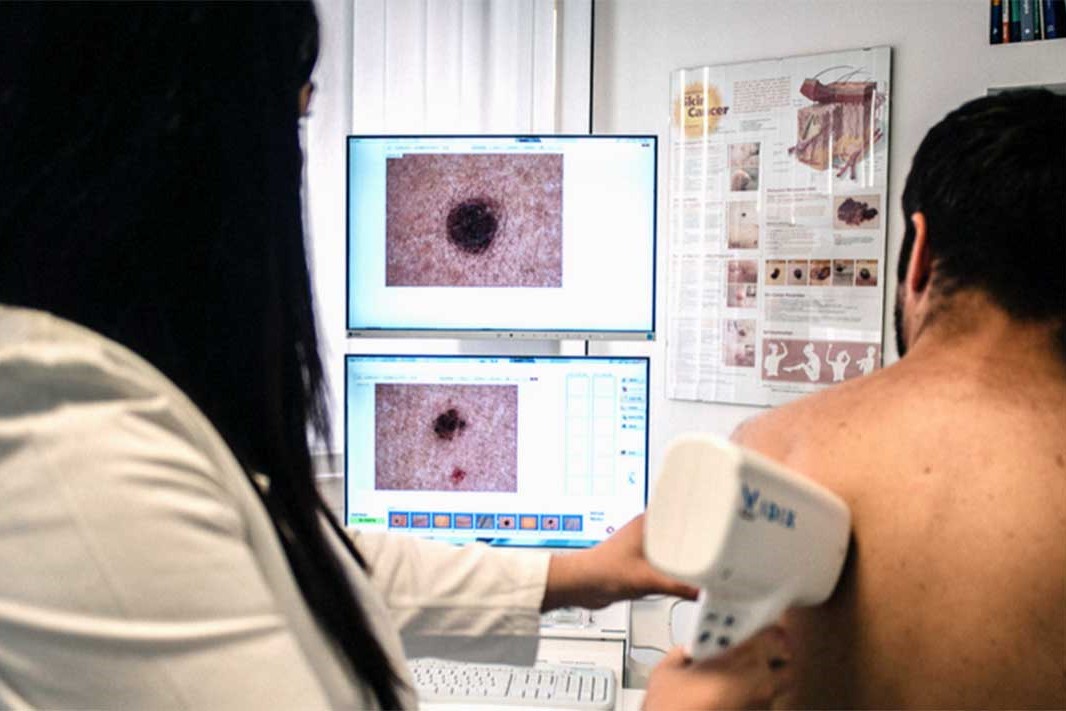
During the dermatological examination, during the objective examination, the doctor will use the
- hand-held dermatoscope, a special lens that makes it possible to enlarge and visualise the deep structures of the spots being examined;
- videodermatoscope, a latest-generation piece of equipment, also available at the La Madonnina Treatment Centre, which makes it possible to
- enlarge skin spots up to 100 times;
- visualise them on one or more screens;
- archive them for monitoring over time: so-called ‘mole mapping’.
In any case, the experience of the specialist is fundamental: it is this, combined with the quality of the instruments and images obtained, that leads to the diagnosis.
How to treat melanoma
The most appropriate therapy is determined by the oncology specialist according to the stage of the pathology and its spread.
In fact, when the melanoma is still superficial spreading, after an early diagnosis, therapy allows an average survival of 97% at 5 years.
Differently, the prognosis becomes poorer with spread to the lymph nodes and in the presence of metastases.
The earliest cases of melanoma, which fortunately are the majority, today generally go on to a definitive cure.
However, even for the most severe cases, innovative therapies increasingly lead to cures or chronification, with a good quality of life for the patient.
Melanoma surgery
The main treatment for melanoma is the surgical removal of even suspicious lesions, whereby an uninjured portion of surrounding skin is also included, so as to be sure of the complete removal of the area in question, together with a histological examination.
Removal of the sentinel lymph node
In the case of ulcerated formations or melanomas exceeding 0.8 mm in thickness, indicated by the Breslow method, the lymph node of the nearest lymphatic station, known as the ‘sentinel lymph node’, is also usually removed and biopsied.
In fact, draining the lymph of the body and thus also of the area affected by the melanoma, the lymph nodes are the first to come into contact with any cancer cells.
If histological examinations detect traces of neoplasia in the sentinel lymph node, the patient is referred to the oncologist for possible adjuvant therapy.
Adjuvant therapies for melanoma
In addition to surgery, which remains the primary route, adjuvant therapies, including electrochemotherapy, can be undertaken against melanoma in accordance with AIOM guidelines.
In selected cases of cutaneous spread of melanoma, patients can be subjected to the administration of a drug (bleomycin) at low concentrations intravenously, concomitant with an electrical potential difference originating from some plates, which makes the membrane of the tumour cells more permeable.
This procedure is repeatable and has to be performed under general anaesthesia.
Immunotherapy and molecularly targeted drugs
For the critically ill patient in stage IV or as precautionary therapy in stage III, stages in which radio- and chemotherapy fail, a revolution and a significant prognostic improvement have been represented by the categories of
- immunotherapeutic agents (ipilimumab, pembrolizumab, nivolumab);
- molecularly targeted drugs (vemurafenib, dabrafenib, trametinib, cobimetinib, encorafenib binimetinib etc.).
These are therapies that target the mechanism that prevents the immune system from attacking the tumour.
The causes of melanoma
Compared to other skin diseases such as basal cell carcinoma, the most common form of skin cancer, and spinocellular carcinoma, for which a correlation with sun exposure is known, for melanoma the debate within the scientific community is still open.
Among the different risk factors that favour its occurrence are, in any case, identified
- genetic predisposition and family history, as 4/5% of first-degree relatives of melanoma patients show the same disease;
- skin phototype, i.e. the 7 categories into which the skin is classified according to its colouring (I lighter, VII darker) and its response to ultraviolet radiation. The lowest phototypes, characteristic of people with fair skin, eyes and hair, do not tan and have a lower tolerance to the sun with redness, erythema and a consequently higher risk of melanoma;
- presence of numerous moles (more than 50), as melanoma often arises at or near an acquired or congenital melanocytic mole.
What can be said is that UV radiation can certainly facilitate, especially in those with a predisposition, the development of melanoma, but more than the sum of UV radiation absorbed over time, the danger would be sunburns suffered at a young age and intermittent intense exposure.
Several studies also show an increased risk of melanoma in those who use sunlamps and/or tanning beds especially at a young age.
Melanoma, the importance of prevention
Although, unfortunately, the risk of developing skin cancer during sun exposure cannot be completely eliminated, the doctor reminds us of the importance of following a few simple precautions
- use a sun cream with a filter appropriate to your skin phototype;
- renew sun cream application every 2 hours and always after bathing;
- avoid exposure to the sun during the hottest hours, which could lead to sunburn;
- preferably also wear hats and sunglasses.
Beware of children
The advice given should especially apply to children.
Not only are they particularly susceptible to sunburn, but the cancer process can often result from an alteration that occurred precisely in childhood.
There is, in any case, no absolute contraindication to sun exposure, which is also important for the synthesis of vitamin D, but it is advisable to expose oneself from childhood onwards with moderation and the appropriate precautions, avoiding excesses and burns.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Epidermolysis Bullosa And Skin Cancers: Diagnosis And Treatment
Skin: What To Do In Case Of Folliculitis?
Childhood Psoriasis: What It Is, What The Symptoms Are And How To Treat It
Dermatological Examination For Checking Moles: When To Do It
What Is A Tumour And How It Forms
Rare Diseases: New Hope For Erdheim-Chester Disease
How To Recognise And Treat Melanoma
Moles: Knowing Them To Recognise Melanoma


