Surgery of myocardial infarction complications and patient follow-up
What are the complications of myocardial infarction that are the responsibility of cardiac surgery? Rupture of the papillary muscle (on which the chordae tendineae of the mitral or tricuspid valve grasp), rupture of the free wall of the left ventricle or the formation of an interventricular septal defect are structural complications of myocardial infarction and require surgical treatment, often on an emergency basis
In these cases, the patient presents with heart failure that is often acute and unmanageable with medical therapy; cardiogenic shock may occur within hours and may be precipitated by arrhythmias typical of myocardial ischaemia.
How are the surgical complications of myocardial infarction diagnosed?
The main method of assessing the structural pathology of the heart is ultrasound.
This is a non-invasive method, particularly in its surface (trans-thoracic) form.
Given the complexity of the picture, the often emergency conditions and for more accurate surgical planning, a trans-oesophageal access is almost indispensable, through a specific probe that is introduced through the mouth, after adequate preparation and possible sedation.
Echocardiography (as the ultrasound technique applied to the heart is generally called), thanks to increasingly powerful and refined instruments, in recent years can accurately assess the degree of compromise of the heart chambers, as well as volume and pressure overload.
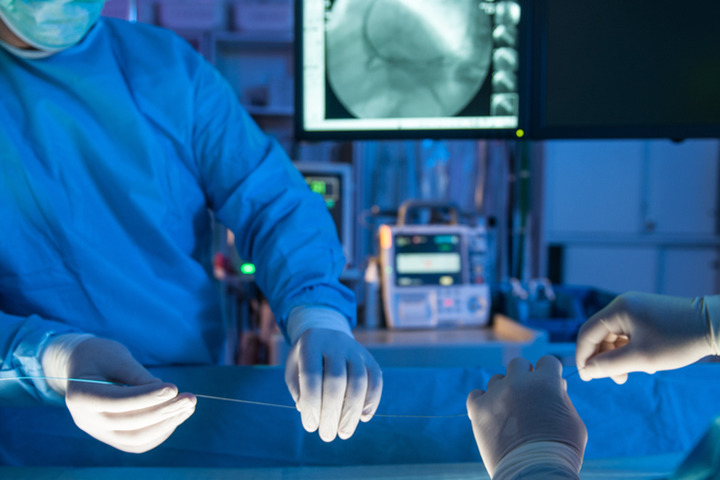
Angiographic evaluation (coronarography) is necessary to confirm the ischaemic origin of the pathology, as well as to plan the possible need for revascularisation of the critical area or neighbouring areas at risk of suffering in the perioperative period.
How is the treatment of surgical complications of myocardial infarction carried out?
The indication for the treatment of surgical complications of myocardial infarction is often made in an emergency, following the acute detection of previously unknown structural alterations or instability of cardiac function.
As a result, the risk of emergency surgery, often of a patient in cardiogenic shock, is weighed against the desirability of haemodynamic stabilisation to allow the operation to be undertaken with reduced risk.
Surgical treatment requires the correction of the structural lesion, in ways that are possible depending on the remaining tissue and function: replacement of the malfunctioning valve or obliteration of a continuous solution of the heart wall or interventricular septum may be required.
The procedure requires extracorporeal circulation assistance during the procedure.
Circulatory assistance may be discontinued at the end of surgery or prolonged for a few days in order to resolve the shock and support the heart in the recovery phase.
Is surgery to treat surgical complications of myocardial infarction dangerous?
Given its emergency nature, surgery is complex and fraught with minor complications such as bleeding, infection, neurological damage, heart failure and peri-procedural infarction.
Other less serious complications consist of pleural inflammation and effusion, atrial fibrillation, pain, poor appetite, fever.
Normally the risk of death associated with this procedure can exceed 30%, but for each individual patient the risk must be assessed, taking into account age, general condition and associated diseases.
Follow-up
At the end of the procedure, the patient is transferred to the intensive care unit, where he/she remains under observation for the time necessary to wean him/her off drugs and any circulatory support systems, before being transferred back to the inpatient ward.
After remission of the general picture, the patient can be discharged from the hospital to be transferred directly to a cardiac rehabilitation centre, where he or she will stay for about 15 days.
Are there any preparation rules?
Prior to surgery, if the patient’s clinical condition permits, a coronarography is performed to assess the state of the coronary arteries and their anatomy, as well as to plan possible myocardial revascularisation at the same time.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Defibrillator: What It Is, How It Works, Price, Voltage, Manual And External
The Patient’s ECG: How To Read An Electrocardiogram In A Simple Way
Signs And Symptoms Of Sudden Cardiac Arrest: How To Tell If Someone Needs CPR
Inflammations Of The Heart: Myocarditis, Infective Endocarditis And Pericarditis
Quickly Finding – And Treating – The Cause Of A Stroke May Prevent More: New Guidelines
Atrial Fibrillation: Symptoms To Watch Out For
Wolff-Parkinson-White Syndrome: What It Is And How To Treat It
Do You Have Episodes Of Sudden Tachycardia? You May Suffer From Wolff-Parkinson-White Syndrome (WPW)
Transient Tachypnoea Of The Newborn: Overview Of Neonatal Wet Lung Syndrome
Tachycardia: Is There A Risk Of Arrhythmia? What Differences Exist Between The Two?
Bacterial Endocarditis: Prophylaxis In Children And Adults
Erectile Dysfunction And Cardiovascular Problems: What Is The Link?
Precordial Chest Punch: Meaning, When To Do It, Guidelines