Unicompartmental prosthesis: the answer to gonarthrosis
The unicompartmental prosthesis is the most suitable solution for treating gonarthrosis, a degenerative and disabling knee disease
Many people are significantly affected by what is called gonarthrosis, or knee osteoarthritis.
This is a form of degenerative disease that begins with an inflammation of the joint (arthritis) that increasingly thins the layers of articular cartilage.
The result is that, over time, due to the degenerative process, the knee bones involved in movement, lacking any layer of cartilage, end up rubbing against each other.
This degenerative knee arthritis leads to a significant worsening of the quality of life, to the point where gonarthrosis can be defined as a disabling disease.
The best solution to gonarthrosis today is the unicompartmental prosthesis
The unicompartimental prosthesis abroad has a 30-year history, while in Italy its application is more recent.
In my practice as a surgeon, I apply the monocompartimental prosthesis in about 70% of cases of gonarthrosis.
Only in the remaining 30% of operations do I implant a total prosthesis.
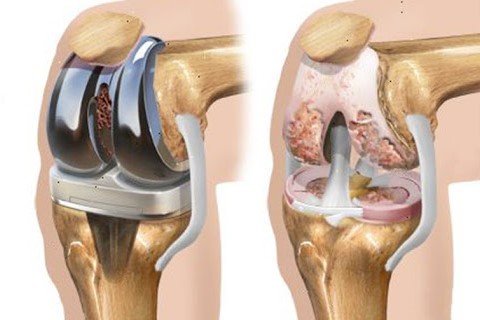
What is a unicompartmental knee replacement
During the degenerative process caused by knee osteoarthritis, the cartilage that protects the bones from being rubbed away gradually thins.
This process in most cases only develops in one compartment.
In these cases, the installation of a unicompartmental prosthesis is therefore recommended.
This is a minimally invasive type of surgery in which only the damaged part of the knee is replaced with a small implant.
Basically, a partial knee replacement is performed.
In fact, this joint can be roughly divided into 3 different compartments:
- patellofemoral: this is located in the front part of the knee, between the kneecap and the femur;
- medial: is on the inside of the knee;.
- lateral: is on the outside of the joint.
By replacing only part of the knee, thus avoiding a total joint replacement, the operation will undoubtedly be less invasive and recovery times will be much faster.
Unicompartmental knee replacement: what the operation consists of
During surgery, the damaged compartment is reconstructed with an implant made of titanium alloy and ultra-high-density polyethylene.
Thanks to these ultra-modern, high-tech materials, it is possible to recreate the native shape of the knee.
In this way, healthy cartilage, bones and ligaments are preserved.
With this type of surgery, very satisfactory results are achieved in most cases.
The success rates of unicompartmental knee replacement are, in fact, very high.
Not to mention that you will experience
- faster recovery;
- less blood loss;
- fewer painful symptoms after surgery.
When the case allows this type of surgery, there are no disadvantages of any kind.
Obviously, if the arthrosis has also affected other compartments and a unicompartmental replacement is performed, the knee relief will only be partial.
Obviously, the choice of the type of surgery is reserved for the orthopaedist, who will have to assess the patient’s specific case in the best possible way.
Who can undergo the operation
Even if arthrosis has developed in only one compartment of the knee, not all patients are suitable for this type of surgery.
There are patients who suffer from chronic inflammatory arthrosis of the rheumatic type for whom this type of operation is not advisable, as well as cases in which the stiffness of the knee has become too great or they have suffered ligament damage.
The ideal patient for this type of operation must be carefully selected on the basis of all relevant medical examinations.
For this reason, it is important to follow a correct procedure that proceeds in steps.
The orthopaedic assessment
A fundamental basis for any type of surgery is a thorough evaluation by a competent orthopaedic surgeon.
The orthopaedic specialist must first assess the patient’s medical history, considering the patient’s general health.
He then also measures the pain felt by the patient and the degree of function of the knee, especially in the area affected by the pain:
- if the pain is concentrated on only one of the affected parts (outer, inner or anterior) the patient might be a candidate for a monocompartmental knee replacement;
- if pain occurs in all parts of the knee, a total joint replacement would probably be more indicated.
Usually, after ascertaining the area affected by the pain, the orthopaedist will perform a physical examination to assess the range of motion and condition of the ligaments.
As we have already mentioned, if he finds injured or fragile knee ligaments, or if he finds knee stiffness in an advanced state, he may more easily opt for a total knee replacement.
Once the orthopaedist has an idea of the knee’s functionality, an initial diagnostic examination using X-rays must be performed to assess the extent of the damage present.
Some cases also prompt surgeons to request a more in-depth diagnostic investigation by means of an MRI in order to assess the condition of the cartilage and ligaments.
Unicompartmental knee replacement: how the operation is performed
With the aim of minimising the invasiveness of the operation, the time the patient has to spend in hospital is kept to a minimum, and ultra-rapid procedures have been developed for this reason.
The patient’s hospitalisation usually starts on the same day as the operation.
Anaesthesia is performed by administering low doses of opiates here as well to ensure a faster recovery.
The actual surgery usually lasts less than 1 hour and does not force the patient to undergo any particularly traumatic procedures.
A robot is also used during the procedure to maximise the precision of the implant and thus the patient’s final functional outcome
An incision is made in the anterior part of the knee, through which a brief analysis of the ligament and compartment situation can be made, and the unicompartmental replacement is confirmed ‘in situ’.
That is, if, as is almost always the case, the conditions revealed by the examinations are confirmed during surgery, a partial replacement is performed, otherwise a change of plan and a total knee replacement can be performed.
Obviously, this will be discussed with the patient before the operation in order not to perform surgery that the person concerned does not approve of.
The first stage of the operation is the preparation of the bone: the residual cartilage of the damaged compartment is machined millimetrically and then the cartilage and bone are replaced with metal liners that recreate the surface of the joint.
The very high-density polyethylene insert is placed between the 2 metal components to create a flawless surface: smooth and flowing.
At this stage, the surgeon assesses the thickness of the insert in order to adapt it to the original cartilage volume of the treated patient.
Post-operation
The patient wakes up in the recovery room where all stages of sedation dissolution are evaluated.
Control X-rays are also taken and then the patient is moved to the recovery room.
Those who undergo this type of knee operation, a mono-compartmental one, tend to experience less pain in the post-operative phase than those who undergo a complete knee replacement.
Less pain and less swelling also often translates into faster rehabilitation times and optimal results: patients usually return home within 1 to 3 days after the operation.
Of course some pain will be experienced after the operation, which can be controlled with medication prescribed by the doctor according to the patient’s profile.
Pain management is also important to improve the psychological aspect of the patient, who, not having any major complaints, will be more committed to rehabilitation.
The orthopaedic surgeon may decide to suggest that the patient use a cane or crutches for the first few days after the operation.
However, it should be noted that it is possible to put weight on the knee right away without fear.
It is obviously necessary to perform rehabilitation exercises, which will be explained to the patient by a competent physiotherapist, in order to restore full function and strength as quickly as possible.
After surgery, the surgeon schedules periodic medical examinations in order to assess the recovery process of the operated joint.
Outcomes and recovery times are very subjective, but usually after a monocompartmental knee operation patients resume all normal activities within 6 weeks after surgery.
Possible complications
Obviously, this type of surgery, like all surgical procedures, also has a number of possible complications, albeit in absolutely low percentages.
The orthopaedic surgeon is obliged to disclose these possible risks to the patient and also to explain the specific measures that will be implemented to avoid complications.
It is possible for blood clots to form in the veins of the legs during this type of surgery, which is why blood thinners, such as low molecular weight heparin, are administered.
In every surgical procedure, there is the possibility of an infection in the skin above the wound or deep within it.
To prevent this, antibiotics are usually administered.
Obviously, the risks associated with anaesthesia must also be considered, although, as we have already mentioned, efforts are made to keep the use of opiates to a minimum.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Wrist Fracture: How To Recognise And Treat It
Carpal Tunnel Syndrome: Diagnosis And Treatment
Knee Ligament Rupture: Symptoms And Causes
Lateral Knee Pain? Could Be Iliotibial Band Syndrome
Knee Sprains And Meniscal Injuries: How To Treat Them?
Treating Injuries: When Do I Need A Knee Brace?
Everything You Need To Know About Fibromyalgia
Knee Cartilage Damage: What It Is And How To Treat It