Bronchiectasis: what are they and what are the symptoms
Bronchiectasis is not often heard of when talking about chronic respiratory diseases, yet it is more common than one might think: it affects about 400 adults per 100,000
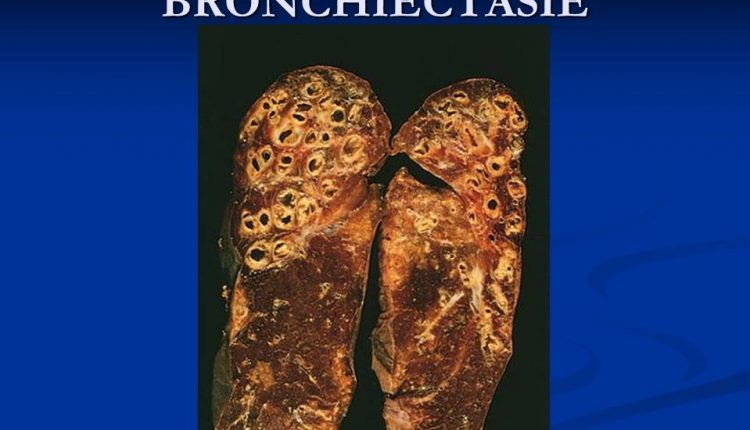
Bronchiectasis is characterised by an abnormal and permanent dilatation of part of the bronchial tree that causes a build-up of catarrh and the frequent development of bronchitis and pneumonia.
What are bronchiectasis
The bronchi are those ‘tubes’ that conduct air into the lungs.
Normally, the bronchi have a standard diameter, but when this increases in width, the bronchi dilate and so-called bronchiectasis develops.
These dilations of the bronchi, therefore, cause a clinical syndrome characterised by an accumulation of catarrh, which is expelled by patients almost every day, with coughing and frequent episodes of bronchitis or pneumonia.
The key to the pathology, in short, lies in the coexistence of a clinical syndrome of phlegm production, coughing, frequent infections and a permanent abnormal dilatation of part of the bronchial tree.
The alarm bells
Coughing, expulsion of phlegm and infections are the symptoms that affect most patients affected by this disease.
However, other manifestations must also be mentioned, such as the presence of blood in the sputum (haemoptysis or haemoptysis), but also shortness of breath, continuous tiredness, night sweats and fever.
These symptoms are defined as ‘accessory’, secondary therefore to the daily production of phlegm, coughing and frequent infections.
However, they must be taken into account because they often occur in association with these three main symptoms.
CT scan of the chest: the tool for diagnosis
Diagnosis first involves a high-resolution CT scan of the chest, which is now the standard for detecting the presence of bronchiectasis.
Patients, therefore, come to the attention of the pulmonologist during a pulmonology examination either because bronchiectasis has been identified during a CT scan of the chest performed for other investigations, or because they present a specific symptomatology.
In the latter case, the pulmonologist will directly request a high-resolution CT scan of the chest to diagnose the disease and assess whether the bronchiectases are clinically significant.
Congenital or acquired: the causes of bronchiectasis
Bronchiectasis can have several causes that are distinguished into congenital or acquired.
There are in fact certain genetic or systemic diseases that can lead to the development of bronchiectasis in the lung, such as cystic fibrosis, primitive ciliary dyskinesia, a pathology that affects the cilia of the bronchi, or the deficiency of a protein called alpha 1 antitrypsin.
Immunodeficiencies, whether primary or secondary, can in fact lead to the establishment of a vicious circle of recurrent infections that, in turn, lead to an anatomical alteration of the bronchus, which is prone to enlargement.
There are also a number of other associations, for example with Crohn’s disease, ulcerative colitis, rheumatoid arthritis or other connective or autoimmune disorders.
And again bronchiectasis in the context of other chronic respiratory diseases such as asthma or chronic obstructive pulmonary disease.
However, one fact should be noted: today, despite the diagnostic technologies available, approximately 40-50% of patients have idiopathic bronchiectasis, i.e., for which no cause can be identified.
In the diagnostic work-up, however, it remains of great importance to carefully assess all possible causes, as many of these are treatable and may require multidisciplinary management or referral to referral centres.
How bronchiectasis is treated
The multiplicity of causes makes the clinical and radiological manifestation of the disease very heterogeneous.
The response to the various treatments, therefore, must also be so. The specialist’s task is to identify what are called ‘treatable disease traits’ in the patient.
The first among these is mucus production: the more phlegm the patient is able to expel, the more the risk of lung inflammation and chronic infection is reduced.
Respiratory physiotherapy is therefore the most important treatment of this disease: for this reason, in the multidisciplinary team of specialists taking care of the patient with bronchiectasis, the respiratory physiotherapist is of great importance, in addition to the pulmonologist.
Other treatable traits are inherent to infection management: antibiotics are used to try to eradicate pathogens from the patient’s bronchiectasis or to try to keep chronic infections under control.
In this case, antibiotics are used by the patient by nebulisation, i.e. by aerosol, for weeks, months or even years depending on the severity of the pathology.
But anti-inflammatory interventions and interventions with immunomodulating drugs such as macrolides may also prove necessary.
Bronchodilators are then used in the event of shortness of breath or obstruction.
Finally, it is important to manage complications, from blood in the sputum to frequent bronchitis.
Multidisciplinary approach: fundamental to the treatment of the disease
The multidisciplinary approach in the management of bronchiectasis is of great importance: the multiplicity of causes and manifestations, in fact, entails the need for collaboration between different specialists.
In addition to the pulmonologist and the respiratory physiotherapist, the microbiologist, who identifies the possible presence of bacteria, fungi or non-tuberculous mycobacteria in order to continue treatment with a specific treatment; the radiologist, who takes over both at the diagnosis stage and in evaluations linked to the presence of blood in the sputum; or the otorhinolaryngologist, because chronic sinusitis is a very frequent comorbidity in patients with bronchiectasis.
The presence of the gastroenterologist is also important, whether in the presence of Crohn’s disease or ulcerative colitis, or comorbidities such as gastro-oesophageal reflux.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Bronchiectasis: How To Recognise And Treat It
Pulmonary Vasculitis: What It Is, Causes And Symptoms
Bronchiolitis: Symptoms, Diagnosis, Treatment
Chest Pain In Children: How To Assess It, What Causes It
Bronchoscopy: Ambu Set New Standards For Single-Use Endoscope
Acute Bronchitis: What Are The Symptoms, How Long Does The Cough Last And How To Treat It
Blind Insertion Airway Devices (BIAD’s)
Oxygen-Ozone Therapy: For Which Pathologies Is It Indicated?
Hyperbaric Oxygen In The Wound Healing Process
Venous Thrombosis: From Symptoms To New Drugs
What Are Bronchiectasis? An Overview
Nasal Cannula For Oxygen Therapy: What It Is, How It Is Made, When To Use It
Pulmonary Emphysema: Causes, Symptoms, Diagnosis, Tests, Treatment
Extrinsic, Intrinsic, Occupational, Stable Bronchial Asthma: Causes, Symptoms, Treatment
A Guide To Chronic Obstructive Pulmonary Disease COPD



