Rheumatoid arthritis: initial symptoms, causes, treatment and mortality
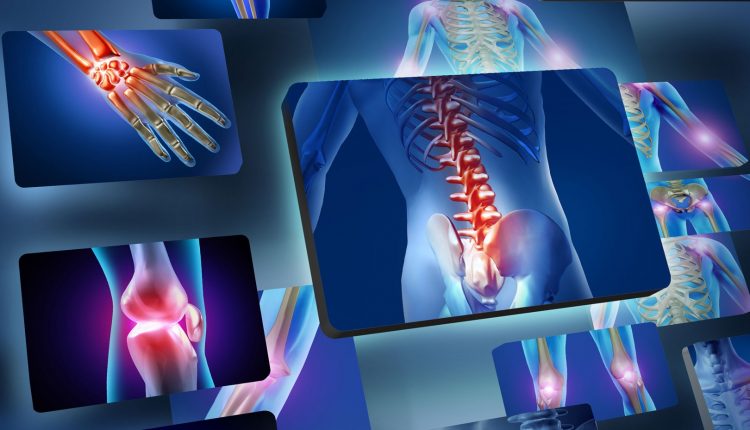
Rheumatoid arthritis (abbreviated ‘RA’; in English ‘rheumatoid arthritis’, hence the acronym ‘RA’) is a chronic, ankylosing and progressive inflammatory polyarthritis with an autoimmune pathogenesis and unknown aetiology, mainly affecting the synovial joints
The affected joints become painful, swollen and deformed over time.
It can also involve other organs and apparatuses such as the lung, serosae, eye, skin and vessels.
It differs from osteoarthrosis in that it initially affects the synovial membrane and not the cartilage; it strikes less frequently and at a younger age than osteoarthritis; women are more affected (3:1 ratio). It affects 1-2% of the population and the number of cases increases with age, with 5% of women over 55 affected.
The onset is mainly observed at the end of adolescence or between the 4th and 5th decade of life; a second peak is observed between the ages of 60 and 70.
An early variant of RA is rheumatoid arthritis of childhood.
What is rheumatoid arthritis?
Rheumatoid arthritis is a chronic systemic inflammatory disease that affects both small and large joints, which become painful, swollen and over time deformed, but can also involve other organs and systems such as the lung, serosae, eye, skin and vessels.
There are two particular and rare variants of rheumatoid arthritis
- Felty’s disease, characterised by enlargement of the spleen, reduction of neutrophil granulocytes on blood count and fever;
- Kaplan’s syndrome: a pulmonary pneumoconiosis.
It most frequently affects women, especially between the ages of 40 and 50.
The prevalence is estimated to be around 1% of the general adult population and familial cases may occur, but more often it is a sporadic disease.
What are the causes of rheumatoid arthritis?
Rheumatoid Arthritis does not have a single, well-determined cause: it is believed that an environmental factor may fool the immune system (molecular mimicry) or modify certain antigens that should be seen as one’s own by the immune system (self), which disrupts immunological tolerance towards certain human proteins, such as joint collagen, causing dysregulation of T-lymphocytes and B-lymphocytes and consequent production of inflammatory cytokines, such as TNF alpha and IL17.
In a high percentage of subjects with Rheumatoid Arthritis, especially in those who carry HLA DR4 or DR1, rheumatoid factor and anti-cyrullinated protein (anti-CCP) antibodies are present, the latter being highly disease-specific.
What are the symptoms and signs of rheumatoid arthritis?
Joints are generally affected symmetrically and additionally; usually the small joints of the hands and feet are affected, but any diarthrodial joint (i.e. with a synovial membrane) can be affected.
Most frequently the inflammation is polyarticular, i.e. affecting more than four joints, and, if left untreated or unresponsive to treatment, can result in bone erosion and deformity.
One of the clinical features of the disease is joint stiffness predominantly in the morning, which may last for several hours.
Spinal involvement is not typical of rheumatoid arthritis although late in the disease there may be involvement of the cervical spine with engagement of the epistropheal tooth and possible involvement of the spinal cord.
As for systemic involvement, the disease can cause pulmonary fibrosis, serositis, vasculitis, nodulosis of the skin and internal organs, episcleritis and scleritis, and amyloidosis.
Diagnosis
Investigations for the diagnosis of the disease and for the detection and staging of organ involvement include, in addition to blood tests for Rheumatoid Factor and anti-CCP antibodies, the assay of inflammation indices such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP).
In addition:
- joint effusion, synovial hypertrophy, bursitis/tenosynovitis, bone erosions:
- joint ultrasound;
- joint radiography;
- joint MRI;
for the study of bone mineral density:
- computed bone mineralometry (MOC).
In the case of extra-articular involvement
- spirometry, DLCO, high-resolution chest CT for studying the lungs;
- echocardiogram for the study of the heart.
Classification criteria
The classification criteria have recently been revised by an international group of experts and require a score greater than or equal to 6 to make the diagnosis considering
- joint involvement:
- large joint involvement (0 points),
- involvement of 2 to 10 large joints (1 pt)
- involvement of 1 to 3 small joints (2 pts)
- involvement of 4 to 10 small joints (3 pts),
- involvement of more than 10 joints (5 pts),
- rheumatoid factor and anti-CCP:
- rheumatoid factor and anti-CCP negativity (0 pt),
- low positivity of rheumatoid factor or anti-CCP (2 pts),
- high positivity of rheumatoid factor or anti-CCP (3 pt,
- inflammatory indices:
- normal inflammatory indices (0 pt),
- altered inflammatory indices (1 pt),
- duration of symptoms:
- duration of symptoms less than six weeks (0 pt),
- duration of symptoms longer than six weeks (1 pt).
Staging, course and treatment
The status of the disease can be identified by analysing the type of lesions on the patient; the course is varied; various pharmacological treatments are possible.
Prognosis and mortality
Joint impairment leads to a limitation of mobility that can result in disability and subsequent premature death.
The course of the disease varies greatly from case to case.
Some patients present with mild symptoms in the short term, but in most the disease progresses throughout life.
Approximately 20%-30% of cases will develop subcutaneous nodules (known as rheumatoid nodules).
Negative prognostic factors include:
- Persistent synovitis.
- Early erosive disease.
- Extra-articular findings (including subcutaneous rheumatoid nodules).
- Positive serological findings for rheumatoid arthritis.
- Serological positivity to anti-CCP antibodies.
- Family history of rheumatoid arthritis.
- Poor functional status.
- Low socio-economic status.
- High acute phase response (erythrocyte sedimentation rate, C-reactive protein).
- Rapid increase in clinical severity.
- Poor response to medication and physiotherapy.
- Sedentary lifestyle.
- Drug use, alcoholism, smoking.
- Poor diet.
- Advanced age.
- Presence of other pathologies (heart disease, diabetes, coagulopathies, obesity…).
A 2006 study claims that rheumatoid arthritis reduces people’s lifespan by about 3 to 12 years.
A 2005 study by the Mayo Clinic noted that sufferers of the condition have a doubled risk of incurring heart disease independent of other risk factors such as diabetes, alcohol abuse, high cholesterol, high blood pressure and a high body mass index.
The mechanism by which rheumatoid arthritis causes this increased risk remains unknown; the presence of chronic inflammation has been proposed as a factor, at least in part, responsible.
Positive responses to therapy may certainly indicate a better prognosis
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Arthrosis: What It Is And How To Treat It
Rheumatoid Arthritis: Staging, Course And Treatment
Juvenile Idiopathic Arthritis: Study Of Oral Therapy With Tofacitinib By Gaslini Of Genoa
Rheumatic Diseases: Arthritis And Arthrosis, What Are The Differences?
Rheumatoid Arthritis: Symptoms, Diagnosis And Treatment
Low-Fat Vegan Diet May Bring Relief From Rheumatoid Arthritis
Bone Callus And Pseudoarthrosis, When The Fracture Does Not Heal: Causes, Diagnosis And Treatment
Septic Arthritis: What Is It, What Causes It And What Are The Treatments



