Tilt Test: what does this test consist of?
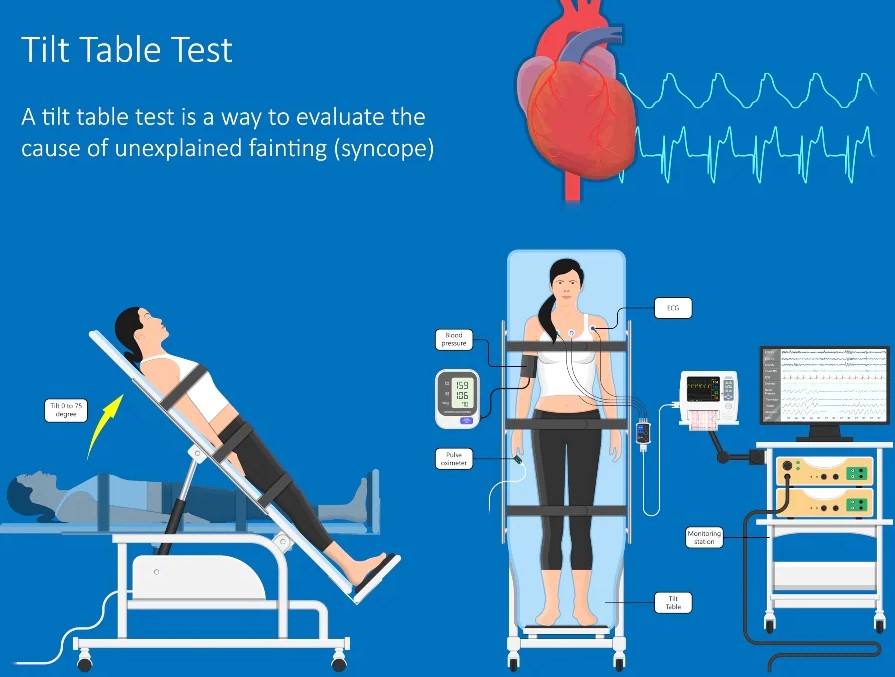
The tilt test is a special diagnostic test that allows the behaviour of the patient’s blood pressure and heart rate to be assessed when moving from a horizontal to a semi-vertical position
The changes in the parameters of the patient, who is positioned on a tilt table, are continuously assessed by means of an electrocardiograph and a blood pressure monitor throughout the test.
How is the tilt test performed?
The patient is positioned and secured, thanks to special straps, on a tilt table, i.e. able to rotate thanks to a motorised mechanism.
The necessary electrodes are attached to the patient to make a continuous recording of blood pressure, ECG, respiratory rate, oxygen saturation and, if indicated, electroencephalogram.
In some cases, sublingual or intravenous medication may be administered to the patient in order to enhance the effect of the prone position.
For this, the insertion of an intravenous access can also be envisaged, thanks to which a rapid administration of the medication is possible should it be necessary.
There are mainly two phases of the tilt test:
- The basal phase, in which the couch remains in a horizontal position for about 5 minutes, thus causing the patient to remain supine;
- The passive phase, in which the couch is tilted by about 60°, so that the patient assumes a semi-vertical position that must be maintained for about 20-30 minutes.
- There may also be a third, pharmacologically enhanced phase, in which the patient in the passive phase is given a drug to trigger the syncopal reflex.
The test is considered completed when syncope or significant changes in blood pressure or heart rate occur or when all phases of the test have been performed without significant responses from the patient.
How should I prepare for the tilt test?
First of all, before performing the test it is important to inform your doctor of any pharmacological therapies you are taking so that he or she can determine whether and how far in advance you should discontinue your medication before the test.
In addition, it is essential to inform your doctor of the presence of any illnesses such as:
- diabetes mellitus
- glaucoma;
- benign prostatic hypertrophy.
In general, as a precautionary measure, it is always a good idea to inform the doctor if you suffer from any kind of disorder or disease.
The patient is also asked to remain fasting and not to drink for at least 2-3 hours before the test.
In many cases, especially when the test is carried out in the morning, the doctor may ask the patient to fast from the previous evening.
Read Also:
Head Up Tilt Test, How The Test That Investigates The Causes Of Vagal Syncope Works
First Aid And Emergency Interventions: Syncope
Cardiac Syncope: What It Is, How It Is Diagnosed And Who It Affects
New Epilepsy Warning Device Could Save Thousands Of Lives
Understanding Seizures And Epilepsy
First Aid And Epilepsy: How To Recognise A Seizure And Help A Patient
Neurology, Difference Between Epilepsy And Syncope
Positive And Negative Lasègue Sign In Semeiotics
Wasserman’s Sign (Inverse Lasègue) Positive In Semeiotics
Positive And Negative Kernig’s Sign: Semeiotics In Meningitis
Lithotomy Position: What It Is, When It Is Used And What Advantages It Brings To Patient Care
Trendelenburg (Anti-Shock) Position: What It Is And When It Is Recommended
Prone, Supine, Lateral Decubitus: Meaning, Position And Injuries
Stretchers In The UK: Which Are The Most Used?
Does The Recovery Position In First Aid Actually Work?
Reverse Trendelenburg Position: What It Is And When It Is Recommended
Drug Therapy For Typical Arrhythmias In Emergency Patients
Canadian Syncope Risk Score – In Case Of Syncope, Patients Are Really In Danger Or Not?


