Uterine cancer: causes, symptoms, diagnosis and treatment
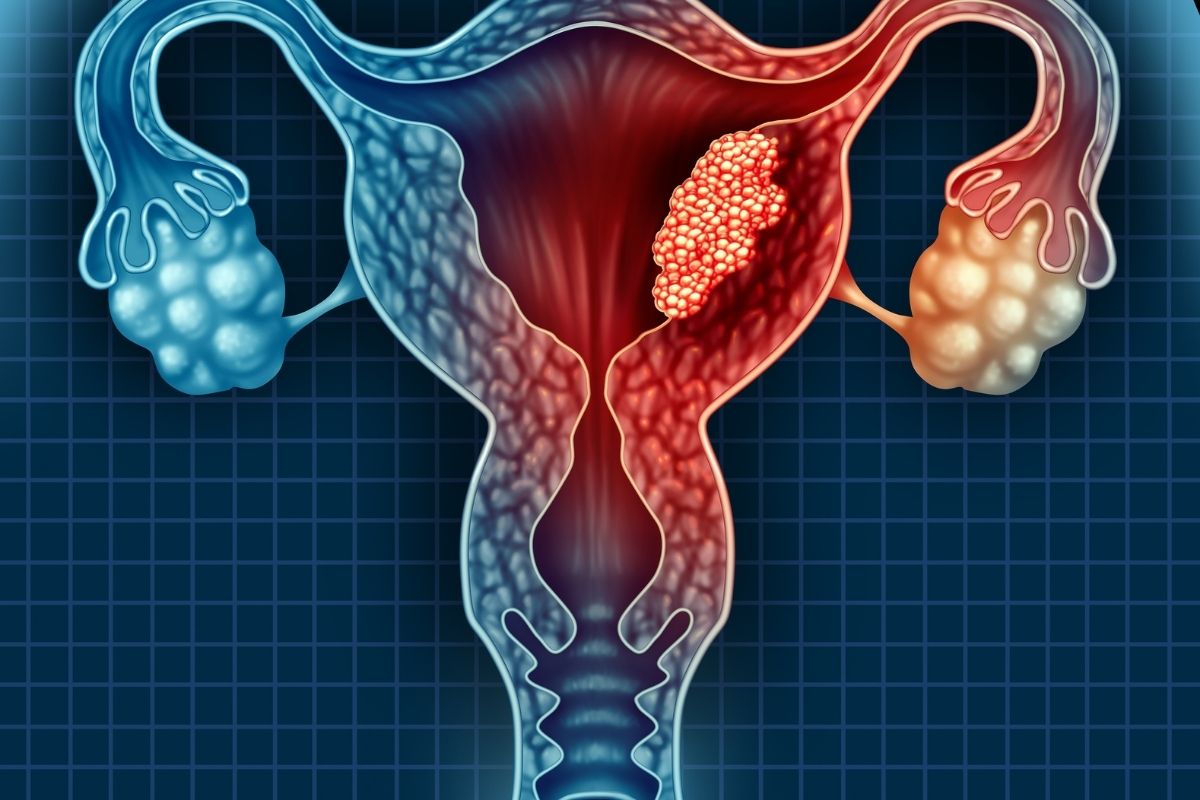
Tumor of the uterus (uterine cancer) – the upside-down funnel-shaped female organ used to welcome the fetus during pregnancy – can affect both the body, i.e. the upper, wider part, and the neck or cervix, i.e. the lower part connected to the vagina
Each of these two parts is made up of different types of tissue, with cells used to perform different functions.
The uterine body is made up of an inner lining layer, called the endometrium.
The endometrium is made up of cells known as epithelial and glandular, and a thicker outer layer called the myometrium, which is made up of muscle cells.
The uterine cervix, in direct connection with the vagina, is instead made up of two portions called endocervix (the one closest to the body of the uterus) and ectocervix or exocervix (the one closest to the vagina).
Uterus, the types of cancer
The cells that cover these two areas are of two different types: the squamous ones are found in the ectocervix and the glandular ones in the endocervix.
The two cell types meet in the so-called transition zone.
Almost all tumors of the uterus originate from endometrial cells and are called endometrial adenocarcinomas (as they affect both the epithelial cells and the glands that make up this tissue).
However, when the tumor develops in the myometrium, it is in the presence of uterine sarcomas.
As far as adenocarcinomas are concerned, there are different types and most of them (80%) are represented by the so-called endometrioid adenocarcinomas.
Other rarer and more aggressive forms are: serous carcinoma, clear cell carcinoma, mucinous adenocarcinoma, undifferentiated carcinoma and carcinosarcoma, which have different risk factors.
As regards, however, tumors of the neck or cervix, they are classified according to the cells from which they originate and are mainly of two types:
- squamous cell carcinoma (about 80% of cervical cancers)
- adenocarcinoma (about 15%).
We speak of squamous cell carcinoma when the tumor arises from the cells that cover the surface of the exocervix and adenocarcinoma when the cancer arises from the glandular cells of the endocervix.
Finally, although less common (3-5% of cervical tumors), there are tumors of the cervix that have a mixed matrix and are therefore defined as adenosquamous carcinomas.
How common is uterine cancer? As far as the uterine body is concerned, endometrial neoplasms make up almost all the cases: they are in fifth place by frequency among the most diagnosed tumors in women.
These are cancers that mainly affect adults after menopause, with a peak incidence over 50 years of age.
With reference to the uterine cervix, however, it can be stated that for a long time this form of cancer has been the most frequent worldwide for women, but recently the situation has significantly changed.
In developed countries the number of cases and that of deaths continue to decrease thanks above all to screening tests – Pap-test and HPV test – which are extremely effective for the early diagnosis of cancer.
Uterus, symptoms of a tumor of the body
In the case of cancer of the body of the uterus, a characteristic symptom is vaginal bleeding, which can be:
- following sexual intercourse
- intermenstrual
- following menopause
If the disease is in an advanced stage, the bleeding can be associated with pelvic pain, which can also affect the lower limbs, and with weight loss (for no apparent reason, therefore basically in the absence of a diet).
Another manifestation of the presence of cervical cancer can be the increase of abnormal vaginal secretions.
The case of cervical cancer is somewhat different
In this case, in fact, the early stages of the cancer are usually asymptomatic and often the eventual manifestations can be linked to other non-tumor pathologies.
In case of symptoms, we witness:
- abnormal bleeding (after intercourse, between periods, or during menopause)
- bloodless vaginal discharge or dyspareunia (pain during intercourse).
Uterine cancer: the causes
As far as endometrial cancer is concerned, estrogen would seem to be the main cause.
It is now almost established that an estrogenic activity not adequately balanced by progesterone (a sex hormone that performs an activity opposite to estrogen) increases the risk of developing this type of tumour.
In the past, in fact, the use of hormonal therapies, aimed at counteracting menopausal disorders, and based exclusively on estrogen, caused a peak in the incidence of endometrial cancer.
Starting from this assumption, all those conditions that increase exposure to estrogens, such as an early start of the menstrual cycle, a late menopause and the absence of pregnancies, are potentially risk factors for the onset of endometrial cancer.
From this point of view, the use of the contraceptive pill, consisting of a balanced dosage of estrogen and progesterone, represents a protective factor.
Further predisposing factors are age (peak incidence after 50 years), obesity, diabetes mellitus and hypertension, which increase the risk of developing cancer by about 3-4 times compared to the general population.
If we talk about cervical cancer instead, the main risk factor is represented by the Human Papillomavirus (HPV) infection which is mainly transmitted sexually.
The condom, in this case, does not completely protect against infection, since the virus can also be transmitted through contact with regions of the skin not covered by the condom.
An early onset of sexual activity, multiple sexual partners or a promiscuous partner can increase the risk of infection, as well as an immunodeficient condition which can be associated with several causes (for example an infection with HIV, the AIDS virus, or a previous organ transplant).
In any case, it is essential to remember that only some of the more than 100 strains of HPV have oncogenic potential and that most women who come into contact with Papilloma are capable of eradicating the infection thanks only to their own immune system without future consequences for health.
Finally, other factors capable of increasing the risk of cervical cancer would appear to be cigarette smoking, the presence of close relatives with this tumor in the family, a diet low in fruit and vegetables, obesity and, according to some studies, even the chlamydial infections.
Diagnosis of uterine cancer
As regards the tumor of the corpus uteri, from a diagnostic point of view, transvaginal ultrasound is the first examination to which the patient is subjected, in order to verify a possible thickening of the endometrial mucosa.
Here, if appropriate, a biopsy will also be performed for subsequent laboratory analysis of a sample of epithelial tissue.
The most used procedure for this purpose is hysteroscopy, which allows the gynecologist to visualize the uterus cavity – through the hysteroscope equipped with a small video camera on the top – and possibly proceed with the biopsy.
Uterine cancer, what exams to do?
Once the on-site diagnosis has been completed, the use of diagnostic imaging (Tac, MRI, Pet) is necessary to evaluate the possible spread of the disease to the lymph nodes or other organs.
Cervical cancer, on the other hand, can be diagnosed in a very early or even precancerous stage if screening with the Pap smear or HPV test is performed regularly.
Based on the results of the tests, the gynecologist will evaluate which intervention to adopt, depending on the risk of the precancerous alteration.
In case of anomalies, it is possible to proceed with colposcopy, an outpatient examination that allows to identify any alterations at the level of the cervix through the magnified view of the tissues.
If necessary, targeted biopsies are also performed at this stage to obtain more in-depth investigations.
When cervical cancer is diagnosed, tests such as computed tomography (CT), magnetic resonance imaging, or positron emission tomography (PET) may be ordered to more accurately evaluate the extent of the tumor.
Evolution
According to the FIGO (International Federation of Gynecology and Obstetrics) classification system, cancer of the corpus uteri, as well as that of the cervix, can be divided into four stages, from I to IV, depending on how widespread it is in the body.
Like other cancers, the lower the stage (and consequently the less common the cancer) and the greater the chances of a cure.
Uterine cancer treatment
Treatment of uterine cancer is influenced by the stage at which it is diagnosed.
There are essentially three possible approaches: surgery, chemotherapy and radiotherapy (sometimes in combination).
Radical hysterectomy, i.e. the removal of the entire organ, is the most frequently applied treatment option.
In cases where the disease is at a more advanced stage, also considering that the neoplasm almost always occurs in menopausal women (hysterectomy involves the loss of fertility), it is also possible to opt for the removal of the ovaries and fallopian tube.
Surgery can be followed by radiotherapy, which in this case can also be internal. Brachytherapy is possible by inserting small eggs through the vagina capable of emitting radiation once they reach the cervix.
In any case, radiotherapy does not preclude the possibility of becoming pregnant after the disease (provided you have undergone fertility preservation treatment).
Chemotherapy, on the other hand, is a procedure reserved for the more advanced forms of cancer of the body of the uterus.
From a pharmacological point of view, where the tumor has particular receptors for estrogen or progestogens – hormone therapy can also be entrusted, by administering substances capable of blocking hormonal activity, considered one of the growth factors of the disease.
Currently, if we think of prophylaxis, there are no specific measures for endometrial cancer but only small tricks that can help reduce the risk.
Good habits
Nutrition and hormonal therapies, for example, play an important role and it will therefore be desirable to follow a healthy diet and maintain normal body weight.
Also perform regular physical exercise and, if it is necessary to use hormone replacement therapy, evaluate the risks and benefits together with the gynecologist, choosing the treatment that best suits your needs.
In the case of cervical cancer, the choice of therapeutic approach is mainly linked to the stage of the disease (but also to more general principles such as the person’s state of health, age and needs).
In the earliest stages, when the tumor is in a pre-invasive stage and the lesions are low-grade, cryosurgery or laser surgery can be used, which use cold or a laser beam respectively to freeze or burn the diseased cells.
These techniques are defined as destructive, as the histological sample is destroyed and is therefore not available for further in-depth analysis.
In cases, instead of moderate or severe dysplasias, the choice may fall on the so-called conization, an operation in which a cone of tissue is removed in correspondence with the lesion without compromising the function of the organ and the possibility of having children.
The most invasive techniques
If, on the other hand, the tumor is more extensive, hysterectomy is performed, an operation that involves the removal of the uterus in its entirety.
Radiation therapy, which targets cancer cells with radiation, is a valid treatment for locally advanced disease, usually in combination with chemotherapy (radiochemotherapy).
To traditional radiotherapy in which the radiation source is external, brachytherapy must also be added, i.e. the insertion into the uterus of small eggs that emit radiation.
Both external therapy and brachytherapy keep the reproductive system intact and, in many cases, do not change the ability to have a normal sexual life.
A third way for the treatment of cervical cancer, reserved however for the advanced or invasive types, is chemotherapy: intravenous administration of various drugs against the tumor, often combined with each other, including cisplatin, paclitaxel, and l antiangiogenic bevacizumab.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Utero-Vaginal Prolapse: What Is The Indicated Treatment?
Urinary Tract Infections: Symptoms And Diagnosis Of Cystitis
Cystitis, Antibiotics Are Not Always Necessary: We Discover Non-Antibiotic Prophylaxis
Polycystic Ovary Syndrome: Signs, Symptoms And Treatment
Vulvodynia: What Are The Symptoms And How To Treat It
What Is Vulvodynia? Symptoms, Diagnosis And Treatment: Talk To The Expert
Accumulation Of Fluid In The Peritoneal Cavity: Possible Causes And Symptoms Of Ascites
What’s Causing Your Abdominal Pain And How To Treat It
Pelvic Varicocele: What It Is And How To Recognise The Symptoms
Can Endometriosis Cause Infertility?
Transvaginal Ultrasound: How It Works And Why It Is Important
Candida Albicans And Other Forms Of Vaginitis: Symptoms, Causes And Treatment
What Is Vulvovaginitis? Symptoms, Diagnosis And Treatment
Polycystic Ovary Syndrome: Signs, Symptoms And Treatment
Radiotherapy: What It Is Used For And What The Effects Are
Ovarian Cancer: Symptoms, Causes And Treatment
Polycystic Ovary Syndrome (PCOS): What Are The Symptoms And How To Treat It
Urethral Stenosis: Definition, Causes, Symptoms, Diagnosis And Treatment
Bladder Prolapse: Do You Suffer From It? Here’s What You Need To Do


