Concussion: what it is, what to do, consequences, recovery time
Concussion consists of a generally temporary and reversible alteration of brain functions caused by brain trauma
These traumas generate a generally reversible and temporary state of confusion in which the nerve centres controlling functions such as memory, balance, and coordination are altered.
The person may momentarily lose consciousness and in some cases a headache may occur.
This is usually a transitory condition, although the effects may last for days or weeks.
It is caused by a very violent single or multiple head injuries, which can occur in a car accident, but also when the person is violently shaken, as in shaken baby syndrome, or during a sporting activity, such as boxing or American football.
The consequences must be carefully monitored.
Causes of concussion
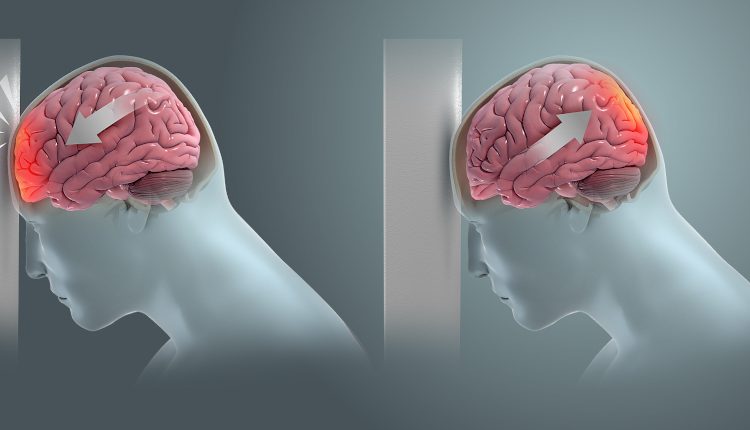
The brain is separated from the bones of the skull by a gelatinous substance (cerebrospinal fluid, also called CSF), which cushions shocks and preserves tissue from injury.
However, under certain circumstances, the violence of a blow or a jolt can momentarily alter the nerve structures that control brain function as the brain ‘slams’ against the skull bones in the opposite direction of the impact of the blow.
Even a simple bump with the violent jerking of the head back and forth can generate trauma with possible loss of consciousness.
The same effect can occur in the case of head impacts, e.g. in a fall, or in the course of sporting activities, such as football or boxing, or in the case of children being violently shaken.
Concussion: who is most at risk?
Infants, children, the elderly and adolescents are more vulnerable to concussions than other age groups and need more time to recover:
- in infants and infants the most frequent cause is shaken baby syndrome;
- in children and adolescents, sports injuries are the most frequent causes;
- in adults, motor vehicle accidents are the most common causes of concussion;
- in elderly patients it is accidental falls.
A number of factors make some people more vulnerable to the effects of a head injury:
- patient aged 65 years or older;
- previous brain surgery;
- conditions involving an abnormality of blood coagulation, such as haemophilia (easier bleeding) or thrombophilia (which makes the blood more prone to clotting);
- therapy with anticoagulant drugs, such as warfarin or low-dose aspirin.
Sports most at risk of concussion
Sports activities that expose individuals to a higher risk of sustaining a concussion include American football, football, rugby, cycling, boxing, and martial arts such as karate or judo.
Concussion symptoms
Concussion symptoms are generally transient and reversible.
They include:
- headache;
- confusional state;
- memory loss (amnesia);
- temporary loss of consciousness;
- dizziness;
- nausea;
- vomiting;
- hyper-sensitivity to light and/or noise;
- double or blurred vision;
- seeing ‘stars’, spots or other visual anomalies;
- loss of coordination and balance;
- numbness, tingling or weakness in legs and arms;
- difficulty speaking;
- ringing in the ears;
- asthenia (tiredness);
- insomnia;
- sleepiness.
The repetition of traumatic events can obviously exacerbate symptoms and lead to deeper and more difficult-to-heal injuries.
Long-term symptoms include memory loss, sleep disorders, sensitivity to light and noise, and mood problems.
In more severe conditions, brain haemorrhage may occur.
Symptoms indicating extreme emergency
Symptoms and signs of emergency include:
- extreme drowsiness, persisting for more than an hour after the injury;
- severe muscle weakness on one or both sides of the body;
- persistent vision problems, unusual eye movements and differently sized pupils of the eyes;
- loss of consciousness;
- extreme difficulty in speaking;
- persistent vomiting or nausea;
- convulsions or seizures;
- bleeding from one or both ears;
- sudden deafness in one or both ears;
- discharge of fluid from the nose or ears (could be cerebrospinal fluid);
- intense ‘dagger-like’ pain in a given spot on the head, which could indicate subdural haemorrhage;
- persistent unconsciousness (coma).
Diagnosis
The doctor makes the diagnosis by means of a medical examination (history and objective examination) and may be aided by CT, MRI and blood tests.
How to recognise a concussion
First, it is important to look at the victim’s head.
Examine the injury and look closely at the patient.
Check for a bleeding head wound.
A concussion is not always visible externally, but often a haematoma (a large bruise) is created under the scalp.
Visible external wounds are not always a good indicator of severity, as some secondary cuts in the scalp bleed profusely, while others, less obvious, such as impact trauma, can cause irreversible brain damage.
It is also important to check whether any behavioural or cognitive symptoms appear.
Since a concussion directly affects the brain, it may also alter the normal behaviour of the patient, who may present for example
- unusual irritability or excitability;
- difficulty concentrating, maintaining logic;
- slowed reflexes and movements;
- difficulty recognising friends and family;
- mood swings, inappropriate emotional outbursts and crying fits.
Assessing the patient’s state of consciousness
While monitoring the victim, you must also check if he is conscious and understand his level of cognitive function.
To check his state of consciousness, use the AVPU rating scale:
A – Is the victim Alert (alert)? Is he/she alert, is he/she looking around? Does he/she respond to your questions? Does he/she react to normal environmental stimuli?
V – Does she/he respond to your Voice? Does she respond normally when you ask her questions and speak to her, even if it is in short sentences or is she not fully alert? Is it necessary to shout for her to respond? A victim may respond to verbal commands but not be alert. If she responds with a simple “huh?” when you speak to her, it means she is verbally responsive but probably not alert.
P – Does she react to Pain or touch? Try pinching her skin to see if she moves a little or opens her eyes. Another technique is to crush or hit the base of her nails. Be careful while using these techniques; you must not cause unnecessary damage. You must only try to get a physical reaction.
U – Is the victim Unresponsive to any stimulus?
What to do if concussion is suspected
1) If the person appears severe (e.g. losing consciousness and bleeding from the head), call the single emergency number immediately without waiting any longer.
If possible, take him/her to the emergency room yourself.
If he/she is not breathing or has no pulse, administer CPR and artificial respiration.
2) Put the subject in the lateral safety position.
If you think the subject may have a spinal cord injury, DO NOT move the subject unless leaving him where he is puts his life at risk.
Stay with the subject until help arrives.
3) Apply ice. To reduce the swelling of a minor injury, you can apply an ice pack to the affected area.
Put it on 2-4 hours apart for 20-30 minutes each time.
Important: Do not place the ice directly on the skin. Wrap it in a cloth or plastic wrap.
Do not put pressure on any head injuries, as you may push bone chips into the brain.
If you cannot get ice, use a bag of frozen vegetables.
4) Have the victim take over-the-counter painkillers. To treat head pain at home, give her paracetamol such as Tachipirin.
Don’t make her take ibuprofen or aspirin because they may cause bruising or aggravate the bleeding.
If you are not sure what you are doing, do nothing and simply wait for medical personnel to arrive, monitoring the victim.
5) Keep the subject awake and focused. If the victim is conscious, keep asking him/her questions.
This serves two purposes: to assess the severity of the injury and to keep the subject awake. By continuing to ask him/her questions, you can observe if changes occur in his/her cognitive state, if he/she can no longer answer a question that he/she was previously able to answer, and so on.
If you notice that his level of consciousness deteriorates, you should consult a doctor.
Here are some useful questions to ask:
What day is it today?
What year is it?
Do you know where you are?
What has happened to you?
What is your name?
What’s your father’s name?
If you’re the victim:
Avoid exertion. In the days following the head injury, you should not engage in sports and other strenuous activities.
During this period, you should also avoid stress.
The brain needs to rest and heal.
Before returning to sports, you should see your doctor.
Do not drive. Do not use a car or ride a bicycle until you feel completely healed. Ask someone to drive you to the doctor’s office or hospital.
Rest. Do not read, watch TV, write, listen to music, play video games or do any other mental task. You must rest both physically and mentally.
Eat foods that help the brain recover. Food is important in helping the brain recover and if it is unhealthy it can further impair the situation. Avoid alcohol after a concussion. Also avoid fried foods, sugars, caffeine, artificial colourings and flavourings. Instead, opt for fruit, vegetables and foods rich in water, vitamins and minerals.
Follow the medical therapy you have been assigned (if your doctor has done so).
If, during convalescence, you suddenly have neurological symptoms, do not underestimate them and seek help.
Recovery times are extremely varied depending on many factors, including:
- severity of the injury
- age;
- general health of the patient.
Concussion can cause a wide range of short- or long-term complications, affecting thinking, feeling, language or emotions.
These changes can lead to memory, communication and personality problems, as well as depression, mild cognitive impairment (MCI) and early onset of dementia.
Other potential complications of a concussion are outlined below:
- Post-concussion syndrome: this is a little-known condition in which concussion symptoms are persistent and may last for weeks or months after the injury.
- Post-concussion seizures: occur days or months after the concussion and may require seizure management with anticonvulsant therapy.
- Epilepsy: the risk of developing epilepsy doubles within the first five years after concussion.
- Second-impact syndrome: can occur when a person is still symptomatic and, before fully recovering from the concussion, suffers another head injury. A second brain injury (or cumulative trauma) can be more dangerous than the previous one. Vascular congestion leads to a sudden and massive increase in intracranial pressure, which can be difficult to control and can cause severe brain damage or death.
- Chronic traumatic encephalopathy (CTE): is an example of cumulative damage. Chronic traumatic encephalopathy, also called boxer’s encephalopathy, is a progressive neurodegenerative disease caused by repeated episodes of concussion. Typical signs and symptoms include a decline in memory, cognitive and physical deficits and behavioural disorders (especially depression, impulsivity, aggression, anger, irritability and suicidal behaviour).
- Chronic traumatic encephalomyopathy (CTE): a small subgroup of individuals with CTE develop a progressive disease characterised by profound weakness, atrophy and spasticity, similar to amyotrophic lateral sclerosis (ALS).
In most cases a concussion does not provide irreversible damage and recovers within a few days, in more severe cases the damage may be irreversible and never fully resolve.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Temporal And Spatial Disorientation: What It Means And What Pathologies It Is Associated With
Neurology, Link Between Traumatic Brain Injury (TBI) And Dementia Examined
Ruptured Brain Aneurysm, Violent Headache Among The Most Frequent Symptoms
Difference Between Concussive And Non-Concussive Head Injuries
Emergency Rescue: Comparative Strategies To Exclude Pulmonary Embolism
Pneumothorax And Pneumomediastinum: Rescuing The Patient With Pulmonary Barotrauma
Barotrauma Of The Ear And Nose: What It Is And How To Diagnose It
Migraine With Brainstem Aura (Basilar Migraine)



