Medest - The pregnant patient management
Author: Mario Rugna, medest118
The management of a pregnant women has been always a challenge for physicians. The different physiology of pregnancy, makes clinical choices and treatment different than in usual adult patient, and needs attentions and practice that override standard care. In emergency medicine, where standards and protocols are a way to think and to act, a change in routine care, together with the time dependency of the decision making process, makes the pregnant patient an effective challenge.
So here is the need of specific guidelines focused on pregnant patient for specific clinical emergency situations.
In this post we discuss two guidelines about the management of a pregnant trauma patient and cardiac arrest in a pregnant women, with an eye of regard on the aspects of the recommendations for prehospital care.
Guidelines for the Management of a Pregnant Trauma Patient (Open Access)
J Obstet Gynaecol Can June 2015;37(6):553–571
Airway
- Every female of reproductive age with significant injuries should be considered pregnant until proven otherwise by a definitive pregnancy test or ultrasound scan. (III-C)
- A nasogastric tube should be inserted in a semiconscious or unconscious injured pregnant woman to prevent aspiration of acidic gastric content.(III-C)
Breathing
- Oxygen supplementation should be given to maintain maternal oxygen saturation >95% to ensure adequate fetal oxygenation. (II-1B)
- If needed, a thoracostomy tube should be inserted in an injured pregnant woman 1 or 2 intercostal spaces higher than usual. (III-C)
Circulation
- Because of their adverse effect on uteroplacental perfusion, vasopressors in pregnant women should be used only for intractable hypotension that is unresponsive to fluid resuscitation. (II-3B)
- After mid-pregnancy, the gravid uterus should be moved off the inferior vena cava to increase venous return and cardiac output in the acutely injured pregnant woman. This may be achieved bymanual displacement (Lateral Uterus Displacement L.U.D.) of the uterus or left lateral tilt (obsolete n.d.r). Care should be taken to secure the spinal cord (if indicated n.d.r.) when using left lateral tilt. (II-1B)
Transfer to health care facility
- Transfer or transport to a maternity facility (triage of a labour and delivery unit) is advocated when injuries are neither life nor limb threatening and the fetus is viable (≥ 23 weeks), and to the emergency room when the fetus is under 23 weeks’ gestational age or considered to be non-viable. When the injury is major, the patient should be transferred or transported to the trauma unit or emergency room, regardless of gestational age. (III-B)
Perimortem Caesarean section
- A Caesarean section should be performed for viable pregnancies (≥ 23 weeks) no later than 4 minutes (when possible) following maternal cardiac arrest to aid with maternal resuscitation and fetal salvage. (III-B)
Take home points on modifications of assessment of trauma patients in presence (or suspect) of pregnancy
-
When indicated a thoracostomy tube should be inserted 1 or 2 intercostal spaces upper than usual.
-
Vasopressors has to be avoided in pregnancy.
-
Perform L.U.D (Lateral Uterus Displacement) to relieve Inferior Vena Cava compression.
-
Transport the severely injuried pregnant patient to an hospital with maternal facility if fetus is viable (≥ 23 weeks).
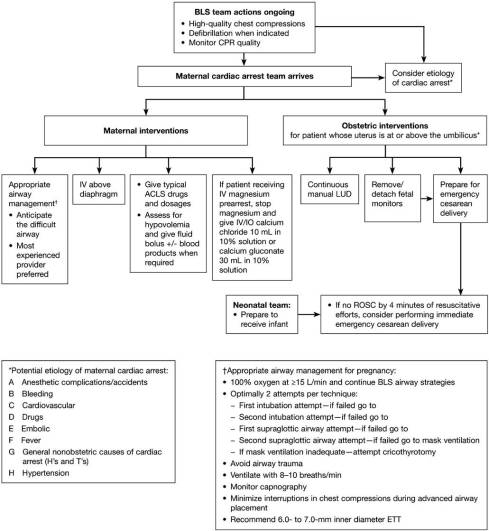
Cardiac Arrest in Pregnancy. A Scientific Statement From the American Heart Association (Open Access)
Chest Compressions in Pregnancy
-
There is no literature examining the use of mechanical chest compressions in pregnancy, and this is not advised at this time
-
Continuous manual LUD (left uterus dispalcement) should be performed on all pregnant women who are in cardiac arrest in which the uterus is palpated at or above the umbilicus to relieve aortocaval compression during resuscitation (Class I; Level of Evidence C).
-
If the uterus is difficult to assess (eg, in the morbidly obese), attempts should be made to perform manual LUD if technically feasible (Class IIb; Level ofEvidence C)
![http://circ.ahajournals.org/content/early/2015/10/06/CIR.0000000000000300.full.pdf Cardiac Arrest in Pregnancy]()
Transporting Pregnant Women During Chest Compressions
-
Because an immediate cesarean delivery may be the best way to optimize the condition of the mother and fetus,this operation should optimally occur at the site of the arrest. A pregnantpatient with in-hospital cardiac arrest should not be transported for cesarean delivery. Management should occur at the site of the arrest (Class I; Level of Evidence C). Transport to a facility that can perform a cesarean delivery may be required when indicated (eg, for out-of-hospital cardiac arrest or cardiac arrest that occurs in a hospital not capable of cesarean delivery)
Defibrillation Issues During Pregnancy
-
The same currently recommended defibrillation protocol should be used in the pregnant patient as in the nonpregnant patient. There is no modification of the recommended application of electric shock during pregnancy (Class I; Level of Evidence C).
Breathing and Airway Management in Pregnancy
Management of Hypoxia
- Hypoxemia should always be considered as a cause of cardiac arrest. Oxygen reserves are lower and the metabolic demands are higher in the pregnant patient compared with the nonpregnant patient; thus, early ventilatory support may be necessary (Class I; Level of Evidence C).
- Endotracheal intubation should be performed by an experienced laryngoscopist (Class I; Level of Evidence C).
- Cricoid pressure is not routinely recommended (Class III; Level of Evidence C).
- Continuous waveform capnography, in addition to clinical assessment, is recommended as the most reliable method of confirming and monitoring correct placement of the ETT (Class I; Level of Evidence C) and is reasonable to consider in intubated patients to monitor CPR quality, to optimize chest compressions, and to detect ROSC (Class IIb; Level of Evidence C). Findings consistent with adequate chest compressions or ROSC include a rising Petco2 level or levels >10 mm Hg (Class IIa; Level of Evidence C).
- Interruptions in chest compressions should be minimized during advanced airway placement (Class I; Level of Evidence C).
Arrhythmia-Specific Therapy During Cardiac Arrest
- No medication should be withheld because of concerns about fetal teratogenicity (Class IIb; Level of Evidence C).
- Physiological changes in pregnancy may affect the pharmacology of medications, but there is no scientific evidence to guide a change in current recommendations. Therefore, the usual drugs and doses are recommended during ACLS (Class IIb; Level of Evidence C).
Epinephrine and vasopressine
- Administering 1 mg epinephrine IV/IO every 3 to 5 minutes during adult cardiac arrest should be considered. In view of the effects of vasopressin on the uterus and because both agents are considered equivalent, epinephrine should be the preferred agent (Class IIb; Level of Evidence C).
Fetal Assessment During Cardiac Arrest
- Fetal assessment should not be performed during resuscitation(Class I; Level of Evidence C).
Delivery durin cardiac arrest
- During cardiac arrest, if the pregnant woman (with a fundus height at or above the umbilicus) has not achieved ROSC with usual resuscitation measures with manual uterine displacement, it is advisable to prepare to evacuate the uterus while resuscitation continues (Class I; Level of Evidence C)
- PMCD (Peri Mortem Cesarean Delivery) should be strongly considered for every mother in whom ROSC has not been achieved after ≈4 minutes of resuscitative efforts (Class IIa; Level of Evidence C).
-
If maternal viability is not possible (through eitherfatal injury or prolonged pulselessness), the procedure should be started immediately; the team doesnot have to wait to begin the PMCD (Class I; Level of Evidence C).
-
Assisted vaginal delivery should be considered when the cervix is dilated and the fetal head is at an appropriately low station (Class IIb; Level ofEvidence C)
Take home points for resuscitation in trauma patient:
-
The utilization of mechanical chest compressors is not recommended.
-
Continuous LUD should be performed during resuscitation.
-
No modification in energy level when electrical therapy is needed.
-
No modification in timing and doses of ACLS drugs.
-
Fetal assessment is not indicated during resuscitation.
-
Peri Mortem Cesarean Delivery (PMCD) has to be performed without delay and at the site of cardiac arrest (no transport is indicated), after 4 minutes of ineffective resuscitation attempts.