
Aggressive Drunk Patient on Ambulance
A drunk patient onboard the ambulance is not the goal of EMTs and paramedics on duty. However, especially during night shifts, it can happen to face such scenarios.
Almost every emergency medical professional had to treat a drunk patient, at least one time. This case study happened in Israel and the protagonist is a volunteer for the national ambulance service in the centre of Israel. Even if Israel is famous for its violent scenarios, because of terrorism and hostile population groups, the protagonist works in non-violent environments.
The incident: the aggressive drunk patient
The factual information is presented as the sequence of events occurred and as information became available.
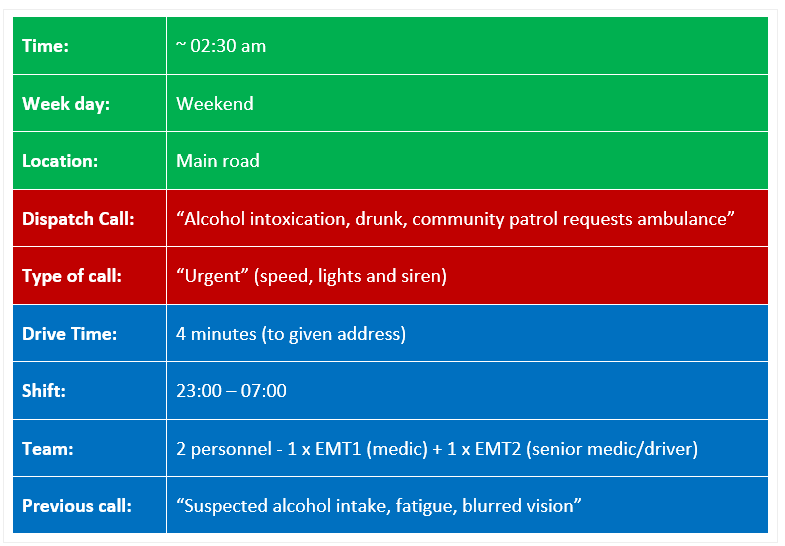
Based entirely on the above information provided by the dispatcher, we dispatched to the call. Having just attended to a similar previous call we were relatively relaxed and not expecting anything extraordinary. The fact that the “community patrol” (security) was on-scene and had requested an ambulance, also indicated less reason for any concern.
We were rather puzzled by the address given as it was an address on the main road which has few residential house addresses. While driving on the main road, we were looking for the community patrol orange flashing lights and saw them from a distance on the main road, as well as blue police lights.
We arrived at a motor vehicle accident at the traffic light where one vehicle had driven into the back of another at a red traffic light. While exiting the ambulance with equipment, we were briefed by a policeman who reported on only one person requiring assistance – the driver of the vehicle that collided with the stationary vehicle.
A quick visual assessment of occupants from the other vehicles verified that there were no other injuries. The policeman who briefed us said that the driver was “totally drunk”, “smells of alcohol” and “was walking around cursing before he noticed the police, then got back into the driver’s seat to sleep”.
The driver did not react to name calls but did react to pain which was met with slurred curses. We transferred the driver to the ambulance to check vitals since there were no visual injuries. The driver was clearly bothered by the ambulance team’s attention and preferred to “sleep”.
Once we determined that hemodynamics and breathing were stable, the ambulance driver prepared for an evacuation by getting into the driver’s seat in the ambulance, leaving me alone with the drunk patient. Since the police suspected drunken-driving (a criminal offence), a policeman was to escort us and the suspected drunk patient in the ambulance to the hospital.
When the drunk patient saw the policeman entering the ambulance he became violent, lashed out and attempted to exit the ambulance. The policeman, the ambulance driver and I managed to restrain the drunk patient without sustaining any blows or injuries. We initially restrained the driver by pinning him down forcibly on the stretcher with our weights, then explained the consequences of attacking a policeman and ambulance team member.
The drunk patient verbal agreement to refrain from any form of further violence was sufficient to prevent the use of physical methods such as handcuffs and/or triangular bandages. The drive to the hospital (8mins), as well as admission to the hospital, passed without further violent incident. Blood was taken with a little verbal resistance, and the ambulance team left after completing the standard required reports.
Analyzing this incident in retrospect, I think that there were a number of clues that were missed and that could help derive best practices which could be implemented to ensure team safety. There were also a number of moral dilemmas which flashed my mind during the incident. I think that proper training, briefings and discussion about the dilemmas might have helped me act with complete confidence instead of wasting time weighing options. These will follow in the next “analysis” section.
Case study analysis: drunk patient onboard the ambulance
The analysis of my case study includes both general best-practice ideas and lessons learned from the incident presented, as well as insight into the specifics of the incident itself.
Routine is the security pitfall. Anyone who has ever dealt in any type of security or safety issues knows that “routine” poses danger. In order to remain alert and function as perfectly as possible, one has to be very wary of the carelessness that comes with a “routine” mindset. It is obviously not by chance that I included the “previous drunk call” in the incident section.
While many emergency calls might follow a type of pattern, each call can potentially develop into something totally unexpected, especially regarding safety/violence. I feel that the “previous drunk call” that we attended to right before the drunk patient call dulled our senses. We were in a completely relaxed mindset and thus missed some of the clues that I feel that we should have noticed on time. We could expect a drunk patient.
By definition, ambulance work demands attentiveness, alertness and also continuous weighing up of “what could go wrong”. I’m not calling for hysteria but rather for an emergency crew to recognize the “routine” pitfall and remain alert, to see each call as a unique incident that requires all the probing and mind-checks necessary to function well.
Seek information. If there is any information that does not make sense, no matter how seemingly insignificant – probe it. We are all aware that there are communication breaks between the callers to dispatchers to teams. The information relayed is not always the information perceived by dispatchers and then additionally relayed and perceived by the teams. In retrospect, the given address should have been a red flag signalling that we were not on just another “drunk club call” but something else – in this case, a motor vehicle accident.
The mindset and mind-checks for a motor vehicle accident are very different from a simply drunk patient. We had 4 entire minutes to explore and obtain this important information but missed it due to (a) routine and (b) leaving something a little puzzling unsolved.
Reassess all the time. Once we saw the blue police lights, we should have connected the dots: main road + police + cars + “drunk” = motor vehicle accident involving a drunk driver. I know that both my partner and I were fixed on simply a drunk patient. It is not criminal to be drunk but drunken driving is criminal.
Had we reassessed or even simply voiced the idea, I am quite sure that we would have arrived on-scene more alert and ready for potential dangers.
What If? This is one of the crucial lessons learned from this case study and it has served me well ever since. Ask many “What ifs?”. Specifically, in this particular case, had I asked myself, “What if the drunk patient is not asleep?”, a lot of the drama might have been avoided. I have no doubt that the policeman who briefed our team was convinced that the driver really was asleep. His intentions were pure but both team members did not question it. We should have. In retrospect, the driver was drowsy-drunk but definitely not asleep. He was trying to avoid police questioning by pretending to be asleep.
The ambulance driver is last. The ambulance driver should be the last team member to take the position before evacuation. In the case presented, we were only two team members and the driver took position before all the ambulance doors were closed and all passengers seated. In effect, I was left alone with the patient in the back while a policeman still to enter the ambulance. The violent incident occurred at the exact moment that the policeman was getting into the ambulance, meaning that the ambulance driver’s assistance was not available. It would have been far easier for two team members and the policeman to restrain the drunk driver.
Minimize confrontation. I am fairly convinced that the drama that ensued might have been avoided if both the policeman and ambulance crew had been trained to try and keep confrontation to a minimum. In this particular case, since the drunk patient was relatively drowsy (but not asleep as illustrated above), it would have been wiser than the policeman either sit next to the driver or sit in the paramedic seat after getting into the ambulance via the ambulance’s side door, thus avoiding eye contact and full frontal presence.
Drunk patient on the ambulance – The conclusion
Moral dilemmas. All the previous sections in this assignment have omitted personal, human and emotional aspects of the incident. These also include some dilemmas as follows:
1. Judgement – before evacuation and during treatment details about the incident and driver became available: young driver, previous serious traffic offences, substance abuse etc. There were two other motor vehicles connected to this incident whose occupants might’ve been my children. I found myself not only judging the driver for drunken driving (unverified of course at the time of interaction), but also for being a serious danger/threat much closer to home i.e. my children, family. etc. It would be dishonest to say that I didn’t judge the apparent drunk patient, especially after seeing the trauma experienced by the young occupants of the other vehicles. I did judge the driver’s behavior to be criminal and do remember thinking that I was glad that the police were on-scene to deal with it. I do remember being acutely aware or thinking that I’m dealing with an apparent criminal, but at the same time, I remember making a conscious note to act professionally, represent my organization honourably and act appropriately. I managed all three.
But then, things changed.
2. Anger – When the driver turned violent and lashed out, I was literally being attacked. Arguably, it was not personal, but it was. Just a minute or two previously, I had had flashes of this individual hurting my children/family. Being drowsy-drunk, the driver was slow and ineffective and the policeman and I swiftly restrained him. I felt tinges of anger building during the confrontation but the violent confrontation ended quickly. I have recounted this episode many times and can safely say that I did not act out of anger. It was there somewhat, that I do know, but there was either not enough time for it to mature into action, or, I have a conscious block that does not allow anger to acting in a situation as the above. I am honestly not sure which it is, or perhaps, a combination of both. I felt pretty secure during the incident, partly because of the presence of a policeman and partly because of the martial art training.
I often play through different scenarios of the same incident and wonder how I could better manage future incidents. There is no one answer and only through discussion, debate and experience of others can one adequately prepare for incidents of this nature – the exact reason I am participating in this course. I think that each situation, the circumstances and events, the organizations and populations are different and thus, one has to be confident in one’s approach, your organization and support mechanisms. This is definitely a topic for discussion which I did not receive during my training and it should be included in syllabi or at least workshops or courses like this one. I pray for the safety of all medical teams and welcome any and all feedback.



