Faecal calprotectin: why this test is performed and which values are normal
Faecal calprotectin: this is a very important test for diagnosing and following numerous inflammatory bowel diseases such as Crohn’s disease and ulcerative rectocolitis
Calprotectin is a protein that binds substances such as calcium and zinc
It is found almost everywhere in the body, but is mainly present in white blood cells called neutrophil granulocytes and, albeit in lower concentrations, in monocytes and macrophages.
In the event of inflammation of the gastrointestinal tract, white blood cells are drawn into the intestine and there release the chemical mediators of inflammation and calprotectin.
As a result, the concentration of calprotectin in the faeces increases.
Within the white blood cells, calprotectin also has a high antimicrobial activity, counteracting the growth of bacteria and fungi.
It can therefore be considered an indirect marker of intestinal inflammation.
The concentration of calprotectin in faeces is determined by an enzyme immunoassay (ELISA)
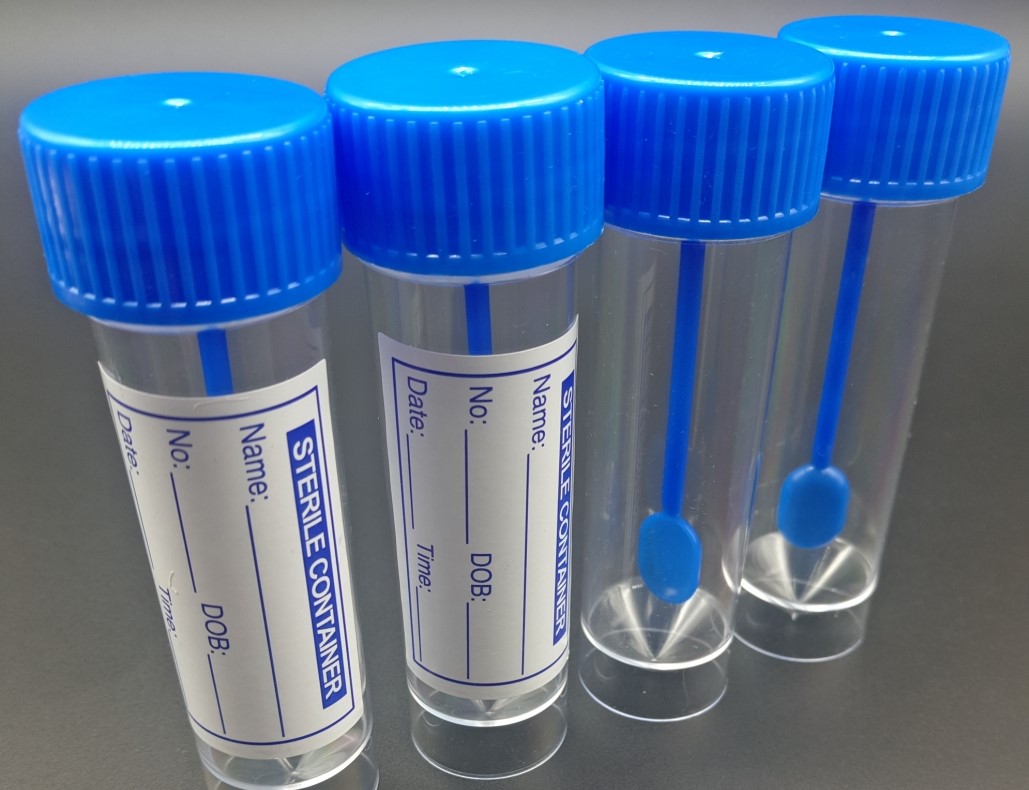
On a small amount of faeces, uncontaminated by water or urine and placed in a clean jar, the laboratory collects the correct amount of material to work with, using a specific device (test tube) fitted with a cap with a rod.
The rod is fitted with a screw-shaped thread into which, by immersion, the sample will adhere.
When closing the device, the rod, with the sample attached, is immersed in an extraction liquid on which the test is performed.
Faecal calprotectin measurement may be required in the presence of typical symptoms of a gastrointestinal inflammation: diarrhoea or haemorrhagic diarrhoea, abdominal cramps or pain, fever, weight loss, rectal bleeding, weakness.
Since these symptoms are also present in non-inflammatory intestinal diseases, the presence of an inflammation or infection in the intestines can be assessed by detecting an increased concentration of calprotectin in the faeces.
Before the test is carried out, it is preferable to abstain from strenuous physical activity (two days prior to the test), to avoid collecting the sample during the menstrual period or in haemorrhagic intestinal situations (haemorrhoids).
The doctor may require discontinuation of therapy with non-steroidal anti-inflammatory drugs (including aspirin) and gastric acidity inhibitors. Fasting is not required.
Normal values vary depending on the method used.
In general, its concentration is higher the more severe the inflammation.
In the laboratory, the reference ranges are divided into:
- Negative less than (<) 50 µg/gr
- Weakly positive 50 – 120 µg/gr
- Positive above (>) 120 µg/gr
High concentrations of calprotectin in faeces are mainly found in chronic inflammatory bowel diseases (IBD) such as Crohn’s disease and ulcerative rectocolitis, making this protein useful as an indicator of inflammation.
In these cases, the clinician usually requires more in-depth investigations such as an endoscopic examination (colonoscopy, sigmoidoscopy, ileoscopy) or ultrasound of the abdomen.
For patients who have already been diagnosed with chronic inflammatory bowel disease, the examination may be useful to assess its severity, to suspect a flare-up, and to monitor the disease’s progress over time.
An increase in faecal calprotectin may also occur in some infections of bacterial origin (perform a co-culture at the same time).
In this case there will be a decrease in the calprotectin concentration at the time the infection ends
Another cause of increase is tumours of the digestive tract: in particular, the combination of the calprotectin assay with faecal occult blood detection increases sensitivity as a screening test for colorectal cancer.
Even in the presence of the gastro-intestinal complaints that prompted the doctor to prescribe the test, the detection of a low concentration of calprotectin in the faeces is usually a sign that these complaints are due to a non-inflammatory bowel disease, such as a viral infection, irritable bowel syndrome or coeliac disease.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Faecaloma And Intestinal Obstruction: When To Call The Doctor
Pinworms Infestation: How To Treat A Paediatric Patient With Enterobiasis (Oxyuriasis)
Intestinal Infections: How Is Dientamoeba Fragilis Infection Contracted?
Gastrointestinal Disorders Caused By NSAIDs: What They Are, What Problems They Cause
Intestinal Virus: What To Eat And How To Treat Gastroenteritis
Train With A Mannequin Which Vomits Green Slime!
Pediatric Airway Obstruction Manoeuvre In Case Of Vomit Or Liquids: Yes Or No?
Gastroenteritis: What Is It And How Is Rotavirus Infection Contracted?
Recognising The Different Types Of Vomit According To Colour
Irritable Bowel Syndrome (IBS): A Benign Condition To Keep Under Control
Colitis And Irritable Bowel Syndrome: What Is The Difference And How To Distinguish Between Them?
Irritable Bowel Syndrome: The Symptoms It Can Manifest Itself With
Experts Call For Changes To The Way IBS (Irritable Bowel Syndrome) Is Diagnosed
What Is Dolichosigma? Causes, Diagnosis And Treatment Of The Condition
Black Stools And Melena: Causes And Treatment In Adults And Infants
Faecal Colour: Normal And Pathological
What Is Faecal Incontinence And How To Treat It


