What is cholecystitis? Symptoms, diagnosis and treatment
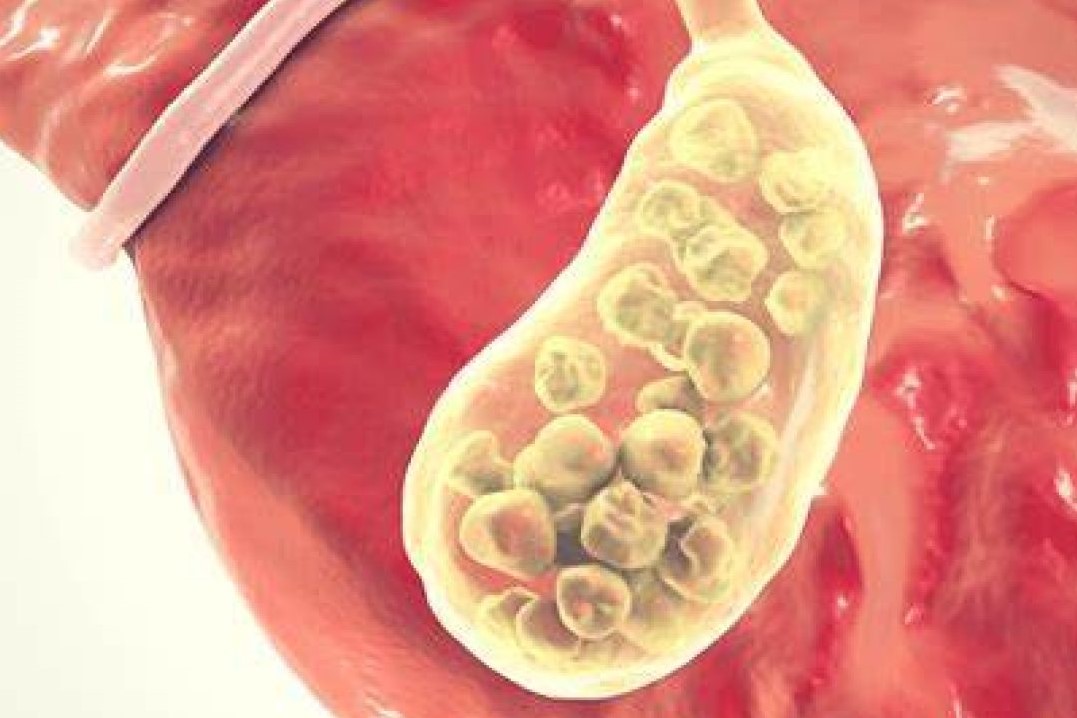
Several disorders affect the biliary system and interfere with normal drainage of bile into the duodenum. Cholecystitis is the acute or chronic inflammation of the gallbladder
There are two classifications of cholecystitis:
- Calculous cholecystitis. In calculous cholecystitis, a gallbladder stone obstructs bile outflow.
- Acalculous cholecystitis. Acalculous cholecystitis describes acute inflammation in the absence of obstruction by gallstones.
Calculous and acalculous cholecystitis have different origins
- Obstruction. Calculous cholecystitis occurs when a gallbladder stone obstructs the bile outflow.
- Chemical reaction. Bile remaining in the gallbladder initiates a chemical reaction; autolysis and edema occur.
- Compression. Blood vessels in the gallbladder compressed, compromising its vascular supply.
Cholecystitis account for most patients requiring gallbladder surgery
Although not all occurrences of cholecystitis are related cholelithiasis, more than 90% of patients with acute cholecystitis have gallstones.
The acute form is most common during middle age.
The chronic form usually occurs among elderly patients.
The causes of cholecystitis include:
- Gallbladder stone. Cholecystitis is usually associated with gallstone impacted in the cystic duct.
- Bacteria. Bacteria plays a minor role in cholecystitis; however, secondary infection of bile occurs in approximately 50% of cases.
- Alterations in fluids and electrolytes. Acalculous cholecystitis is speculated to be caused by alterations in fluids and electrolytes.
- Bile stasis. Bile stasis or the lack of gallbladder contraction also play a role in the development of cholecystitis.
Cholecystitis causes a series of signs and symptoms:
- Pain. Right upper quadrant pain occurs with cholecystitis.
- Leukocytosis. An increase in the WBC occurs because of the body’s attempt to ward off pathogens.
- Fever. Fever occurs in response to the infection inside the body.
- Palpable gallbladder. The gallbladder becomes edematous as infection progresses.
- Sepsis. Infection reaches the bloodstream and the body undergoes sepsis.
Cholecystitis can progress to gallbladder complications, such as:
- Empyema. An empyema of the bladder develops if the gallbladder becomes filled with purulent fluid.
- Gangrene. Gangrene develops because the tissues do not receive enough oxygen and nourishment at all.
- Cholangitis. The infection progresses as it reaches the bile duct.
Studies used in the diagnosis of cholecystitis include:
- Biliary ultrasound: Reveals calculi, with gallbladder and/or bile duct distension (frequently the initial diagnostic procedure).
- Oral cholecystography (OCG): Preferred method of visualizing general appearance and function of gallbladder, including presence of filling defects, structural defects, and/or stone in ducts/biliary tree. Can be done IV (IVC) when nausea/vomiting prevent oral intake, when the gallbladder cannot be visualized during OCG, or when symptoms persist following cholecystectomy. IVC may also be done preoperatively to assess structure and function of ducts, detect remaining stones after lithotripsy or cholecystectomy, and/or to detect surgical complications. Dye can also be injected via T-tube drain postoperatively.
- Endoscopic retrograde cholangiopancreatography (ERCP): Visualizes biliary tree by cannulation of the common bile duct through the duodenum.
- Percutaneous transhepatic cholangiography (PTC): Fluoroscopic imaging distinguishes between gallbladder disease and cancer of the pancreas (when jaundice is present); supports the diagnosis of obstructive jaundice and reveals calculi in ducts.
- Cholecystography (for chronic cholecystitis): Reveals stones in the biliary system. Note:Contraindicated in acute cholecystitis because patient is too ill to take the dye by mouth.
- Nonnuclear CT scan: May reveal gallbladder cysts, dilation of bile ducts, and distinguish between obstructive/nonobstructive jaundice.
- Hepatobiliary (HIDA, PIPIDA) scan: May be done to confirm diagnosis of cholecystitis, especially when barium studies are contraindicated. Scan may be combined with cholecystokinin injection to demonstrate abnormal gallbladder ejection.
- Abdominal x-ray films (multipositional): Radiopaque (calcified) gallstones present in 10%–15% of cases; calcification of the wall or enlargement of the gallbladder.
- Chest x-ray: Rule out respiratory causes of referred pain.
- CBC: Moderate leukocytosis (acute).
- Serum bilirubin and amylase: Elevated.
- Serum liver enzymes—AST; ALT; ALP; LDH: Slight elevation; alkaline phosphatase and 5-nucleotidase are markedly elevated in biliary obstruction.
- Prothrombin levels: Reduced when obstruction to the flow of bile into the intestine decreases absorption of vitamin K.
- Ultrasonography. Ultrasound is the preferred initial imaging test for the diagnosis of acute cholecystitis; scintigraphy is the preferred alternative.
- CT scan. CT scan is a secondary imaging test that can identify extra-biliary disorders and acute complications of cholecystitis.
- MRI. Magnetic resonance imaging is also a possible secondary choice for confirming a diagnosis of acute cholecystitis.
- Oral cholecystography. Preferred method of visualizing general appearance and function of the gallbladder.
- Cholecystogram. Cholecystography reveals stones in the biliary system.
- Abdominal xray. Radiopaque or calcified gallstones present in 10% to 15% of cases.
Management may involve controlling the signs and symptoms and the inflammation of the gallbladder
- Fasting. The patient may not be allowed to drink or eat at first in order to take the stress off the inflamed gallbladder; IV fluids are prescribed to provide temporary food for the cells.
- Supportive medical care. This may include restoration pf hemodynamic stability and antibiotic coverage for gram-negative enteric flora.
- Gallbladder stimulation. Daily stimulation of gallbladder contraction with IV cholecystokinin may help prevent the formation of gallbladder sludge in patients receiving TPN.
Pharmacologic Therapy
The following medications may be useful in patients with cholecystitis:
- Antibiotic therapy. Levofloxacin and Metronidazole for prophylactic antibiotic coverage against the most common organisms.
- Promethazine or Prochlorperazine may control nausea and prevent fluid and electrolyte disorders.
- Oxycodone or Acetaminophen may control inflammatory signs and symptoms and reduce pain.
Surgical Management
Because cholecystitis frequently recurs, most people with the condition eventually require gallbladder removal.
- Cholecystectomy. Cholecystectomy is most commonly performed by using a laparoscope and removing the gallbladder.
- Endoscopic retrograde cholangiopancreatography (ERCP). ERCP visualizes the biliary tree by cannulation of the common bile duct through the duodenum.
Nursing Management
Management of cholecystitis include the following:
Nursing Assessment
- Integumentary system. Assess skin and mucous membranes.
- Circulatory system. Assess peripheral pulses and capillary refill.
- Bleeding. Assess for unusual bleeding: oozing from injection sites, epistaxis, bleeding gums, petechiae, ecchymosis, hematemesis, or melena.
- Gastrointestinal system. Assess for abdominal distension, frequent belching, guarding, and reluctance to move.
Nursing Diagnosis
Based on the assessment data, the major nursing diagnosis for the patient may include:
- Acute pain related to the inflammatory process.
- Risk for imbalanced nutrition related to self-imposed dietary restrictions and pain.
Nursing Care Planning & Goals
The major goals for the patient include:
- Relieve pain and promote rest.
- Maintain fluid and electrolyte balance.
- Prevent complications.
- Provide information about disease process, prognosis, and treatment needs.
Nursing Interventions
Treatment of cholecystitis depends on the severity of the condition and the presence or absence of complications.
- Pain assessment. Observe and document location, severity (0-10 scale), and character of pain.
- Activity. Promote bedrest, allowing the patient to assume a position of comfort.
- Diversion. Encourage use of relaxation techniques, and provide diversional activities.
- Communication. Make time to listen and to maintain frequent contact with the patient.
- Calories. Calculate caloric intake to identify nutritional deficiencies or needs.
- Food planning. Consult the patient about likes and dislikes, foods that cause distress, and preferred meal schedules.
- Promote appetite. Provide a pleasant atmosphere at mealtime and remove noxious stimuli.
- Laboratory studies. Monitor laboratory studies: BUN, pre-albumin, albumin, total protein, transferrin levels.
Evaluation
Expected patient outcomes are:
- Pain relieved.
- Homeostasis achieved.
- Complications prevented/minimized.
- Disease process, prognosis, and therapeutic regimen understood.
Discharge and Home Care Guidelines
The focus of discharge instructions for patients with cholecystitis is education.
- Education. Patients with cholecystitis must be educated regarding causes of their disease, complications if left untreated, and medical and surgical options.
- Activity. Ambulate and increase activity as tolerated.
- Diet. Consult with the dietitian or nutritional support to establish individual nutritional needs.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Sclerosing Cholangitis: Symptoms, Diagnosis And Treatment
The Dangers Of Raw Or Undercooked Fish: Opisthoriasis
First Time Ever: Successful Operation With A Single-Use Endoscope On Immunodepressed Child
Crohn’s Disease: What It Is And How To Treat It
Wales’ Bowel Surgery Death Rate ‘Higher Than Expected’
Irritable Bowel Syndrome (IBS): A Benign Condition To Keep Under Control
Colitis And Irritable Bowel Syndrome: What Is The Difference And How To Distinguish Between Them?
Irritable Bowel Syndrome: The Symptoms It Can Manifest Itself With
Crohn’s Disease Or Irritable Bowel Syndrome?
USA: FDA Approves Skyrizi To Treat Crohn’s Disease
Crohn’s Disease: What It Is, Triggers, Symptoms, Treatment And Diet
Rare Diseases: Primary Sclerosing Cholangitis


