Cardiac amyloidosis: what it is, what the symptoms are and how to treat it
Cardiac amyloidosis is one of a group of diseases known as amyloidosis. These are rare diseases characterised by the deposition of amyloid, an insoluble protein material that can damage tissues and organs
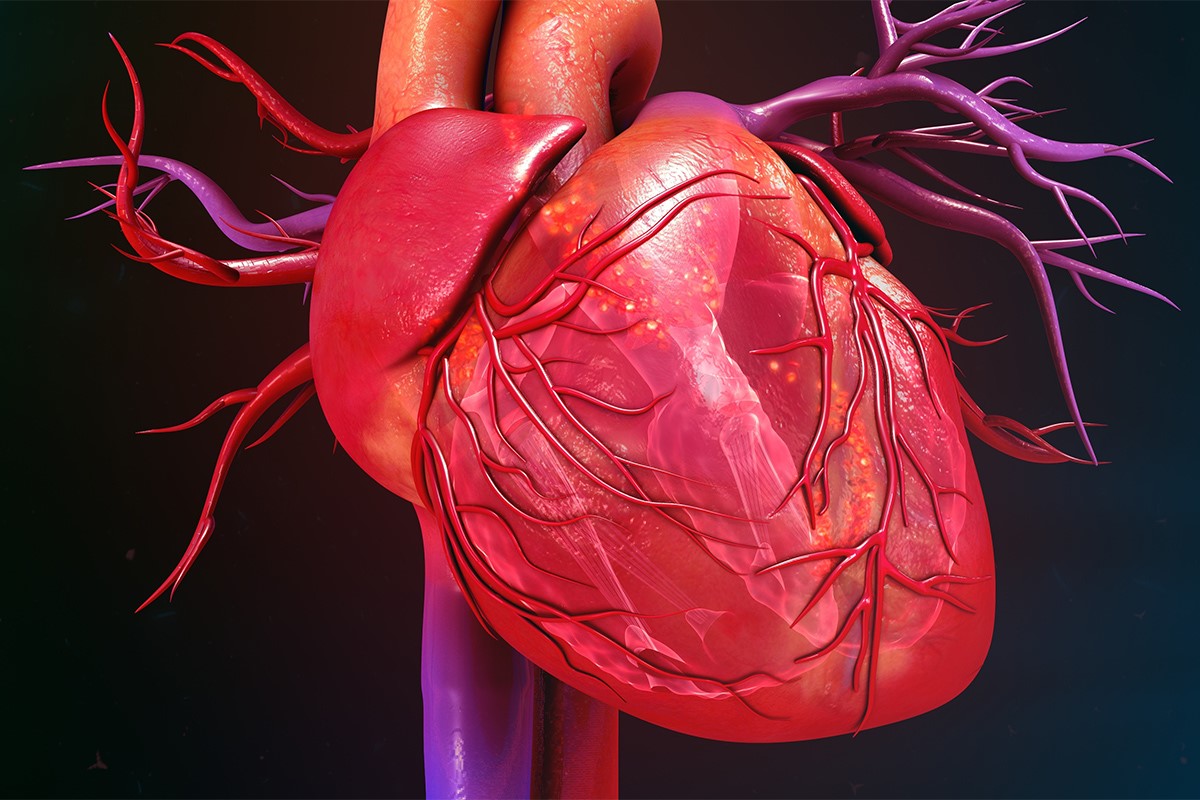
The heart is one of the organs where amyloid is most frequently deposited.
So far, several types of amyloidosis have been described
Those that most frequently involve the heart are:
- Systemic amyloidosis type AL, originating from a plasma cell clone that produces amyloidogenic chains. This pathology responds to specific chemotherapeutic treatments aimed at stopping or slowing down the production of the protein that causes the deposits.
- Hereditary amyloidosis, caused by the accumulation of transthyretin, a protein produced by the liver, which can become amyloidogenic as a result of point mutations and be deposited in various organs and tissues. In particular, in addition to the heart, it can affect the peripheral and autonomic nervous system.
- Amyloidosis caused by the accumulation of unmutated transthyretin.
Cardiac amyloidosis: what is it?
Cardiac amyloidosis is a disease caused by the deposition of amyloid in cardiac tissue, known as the myocardium.
There are two main forms of this disease: immunoglobulin light chain amyloidosis and transthyretin amyloidosis.
The latter condition has two variants: a non-hereditary transthyretin wild type (non-mutated) form and a hereditary transthyretin mutated form.
TRAINING: VISIT THE BOOTH OF DMC DINAS MEDICAL CONSULTANTS IN EMERGENCY EXPO
Symptoms
Cardiac amyloidosis is characterised by an increase in myocardial wall thickness that cannot be explained by any other cause.
Patients with cardiac amyloidosis also present with low voltages on the electrocardiogram.
When hypertrophy cannot be explained, amyloidosis is considered and is therefore a diagnosis of exclusion.
Diagnosis
When amyloidosis is suspected, an electrocardiogram and echocardiography are usually prescribed.
In addition, the BNP and NT-proBNP markers, which indicate the presence of an altered wall, are essential for diagnosing cardiac amyloidosis.
Useful instrumental tests also include MRI and myocardial scintigraphy.
To confirm the diagnosis and characterise amyloidosis, finally, a histological sampling is important.
During the ultrasound scan, the physician will note the increased thickness of the ventricular walls, the interatrial septum and the disproportionate thickening of the atrioventricular valve leaflets, as well as hypertrophy of the right ventricle.
Cardiac amyloidosis: treatment
There are numerous treatments for cardiac amyloidosis.
A number of drugs inhibiting the production of the protein are usually prescribed, which are effective in reducing symptoms and improving patients’ quality of life.
In any case, early diagnosis is crucial for effective treatment.
Cardiac amyloidosis: what is amyloidosis?
The term amyloidosis denotes a group of diseases that are characterised by the accumulation of proteinaceous material called amyloid.
The latter forms deposits in numerous organs. The severity, symptoms and consequences of the disease depend on the organ affected and the type of amyloidosis.
In most cases, the fibrillar deposits are diffuse and can impair the functioning of various organs and tissues.
The diagnosis is confirmed by performing a biopsy test that allows a tissue sample to be analysed under a microscope.
Symptoms vary depending on the type of amyloidosis, as do treatments to manage symptoms and limit amyloid production.
Cardiac amyloidosis: localised or systemic
Amyloidosis is caused by changes in the secondary structure of proteins.
Under normal conditions, proteins are synthesised as a linear sequence of amino acids that fold into a specific shape.
Thanks to this, the protein is able to perform all its functions.
Amyloid proteins derive from a precursor that has been incorrectly processed by cells.
Depending on where the amyloid deposits are localised, it is possible to classify the pathology
- Localised amyloidosis: in this case, the disease affects only one organ or tissue. This is the least severe form of the disease and is more common in older patients or those with type 2 diabetes.
- Systemic amyloidosis: amyloid deposits are found in various organs and have a neoplastic, genetic or inflammatory origin. This form of the disease is quite severe and mainly affects the heart, kidneys, nerves and intestines, leading the organs to progressive failure.
Cardiac amyloidosis: classification
There are different forms of amyloidosis depending on the nature of the proteins that form the fibrillar deposits.
We therefore find:
- Primary amyloidosis (or light-chain amyloidosis, AL)
- Secondary amyloidosis (or acquired amyloidosis, AA)
- Hereditary amyloidosis
- Age-associated amyloidosis (or senile systemic amyloidosis)
Amyloidosis AL
The most common form of systemic amyloidosis is primary amyloidosis (AL).
The disease is caused by the accumulation of fibrils containing immunoglobulin light chains derived from monoclonal plasma cells.
The disease usually results from monoclonal gammopathies and may be associated with multiple myeloma or other lymphoproliferative disorders involving B-cells.
AL amyloidosis is characterised by the presence of fibrillar deposits located at the level of organs that increase until they become clinically manifest.
Symptoms are oedema, weight loss, fatigue and are related to the affected organ as well as the size of the deposit.
In the kidneys, for example, the disease can lead to chronic kidney failure, while when it is found in the heart, it can impair the organ’s ability to supply the body with adequate blood.
The disease particularly affects the liver, kidneys, heart, autonomic and peripheral nervous system.
In rarer cases, it can also affect the lungs, tongue, thyroid, intestines, skin and blood vessels, with signs such as purpura around the eyes, petechiae, ecchymosis, shortness of breath, dizziness, weakness and fluid retention.
Secondary amyloidosis (AA) is less common
It is also called acquired amyloidosis because it can occur as a complication of a disease that causes a persistent inflammatory condition (tuberculosis, leprosy, rheumatoid arthritis) or as a consequence of a neoplastic disease.
Typical places where the accumulation occurs are the spleen, kidneys, liver, lymph nodes and adrenal glands.
Treatment usually starts with treatment of the underlying condition.
Senile systemic amyloidosis is usually associated with the natural ageing of the body.
It is usually found in patients over the age of 60.
Deposits are created and accumulate in the heart and the causes of the formations are not yet known.
Diagnostic tests and specific treatments are also being developed.
Finally, we find hereditary amyloidosis, which is the result of a genetic defect.
Mutations involve certain blood proteins such as, for example, the transthyretin protein, TTR, and can be inherited in an autosomal dominant manner.
This type of amyloidosis affects the nervous system in particular, with deposits also forming in the heart, kidneys and blood vessels.
THE RADIO OF THE WORLD’S RESCUERS? VISIT THE RADIO EMS BOOTH AT EMERGENCY EXPO
Cardiac amyloidosis: the latest studies
In many ways, amyloid remains a mystery to scholars.
This protein accumulates in organs and tissues, progressively altering cell function.
It can affect different areas of the body, causing more or less severe damage.
This altered protein aggregation is at the root of the development of Alzheimer’s disease, although the organ most affected turns out to be the heart.
Cardiac amyloidosis may appear in individuals with no family history or it may have a hereditary basis.
Either way, it causes consequences that can be very serious for the heart, which can go into heart failure.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
What Is Takotsubo Cardiomyopathy (Broken Heart Syndrome)?
Heart Disease: What Is Cardiomyopathy?
Inflammations Of The Heart: Myocarditis, Infective Endocarditis And Pericarditis
Heart Murmurs: What It Is And When To Be Concerned
Broken Heart Syndrome Is On The Rise: We Know Takotsubo Cardiomyopathy
Heart Attack, Some Information For Citizens: What Is The Difference With Cardiac Arrest?
Heart Attack, Prediction And Prevention Thanks To Retinal Vessels And Artificial Intelligence
Full Dynamic Electrocardiogram According To Holter: What Is It?
In-Depth Analysis Of The Heart: Cardiac Magnetic Resonance Imaging (CARDIO – MRI)
Heart Attack Symptoms: What To Do In An Emergency, The Role Of CPR
Heart Attack: Guidelines For Recognising Symptoms
Chest Pain, Emergency Patient Management
Notions Of First Aid, The 5 Warning Signs Of A Heart Attack
Notions Of First Aid: The 3 Symptoms Of A Pulmonary Embolism
Holter Monitor: How Does It Work And When Is It Needed?
What Is Patient Pressure Management? An Overview
Cardiovascular Diseases: What Are Angiology And Vascular Surgery Examinations
Emergency Stroke Management: Intervention On The Patient
Stroke-Related Emergencies: The Quick Guide
The Purpose Of Suctioning Patients During Sedation
Supplemental Oxygen: Cylinders And Ventilation Supports In The USA
Behavioural And Psychiatric Disorders: How To Intervene In First Aid And Emergencies
Fainting, How To Manage The Emergency Related To Loss Of Consciousness
Altered Level Of Consciousness Emergencies (ALOC): What To Do?
Respiratory Distress Emergencies: Patient Management And Stabilisation
Takotsubo Cardiomyopathy: Broken Heart Syndrome Is Mysterious, But Real
Echo- And CT-Guided Biopsy: What It Is And When It Is Needed
Echodoppler: What It Is And When To Perform It
Echocardiogram: What It Is And When It Is Required
What Is Echocolordoppler Of The Supra-Aortic Trunks (Carotids)?
What Is The Loop Recorder? Discovering Home Telemetry
Cardiac Holter, The Characteristics Of The 24-Hour Electrocardiogram
Endocavitary Electrophysiological Study: What Does This Examination Consist Of?
Cardiac Catheterisation, What Is This Examination?
Echo Doppler: What It Is And What It Is For


