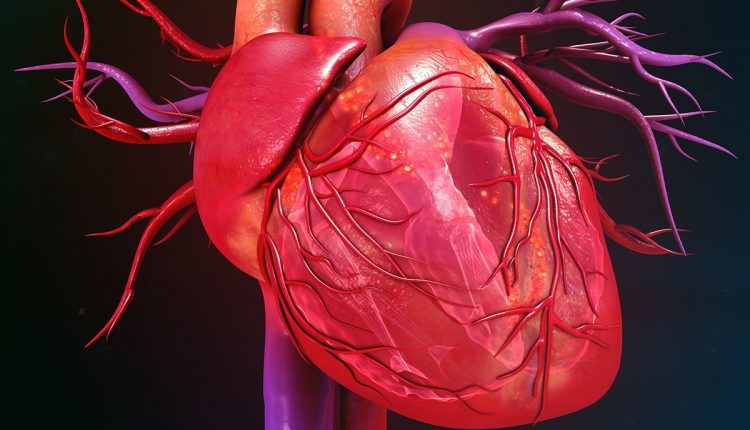
Heart disease: what is cardiomyopathy?
Cardiomyopathy describes any type of heart disease that harms the heart muscle. It makes the heart muscle larger, thicker, or more stiff than normal
This condition makes it hard for your heart to keep a regular electrical rhythm and pump blood.
The effect weakens your heart. It can cause irregular heartbeats called arrhythmias and heart valve problems.
It can also lead to heart failure.
These physical changes can decrease the amount of blood that your heart pumps to your body.
Without enough blood, your organs and body systems can’t function in a normal way.
This article explains cardiomyopathy symptoms, causes, diagnosis, and treatment.
Types of Cardiomyopathy
The cardiomyopathy disorders cause changes that weaken or alter the function of the heart muscle.
However, the exact changes that occur vary by disease type.
The type of disease you have also affects your treatment and outlook.
Common types of cardiomyopathy include:1
- Dilated cardiomyopathy: stretches the heart muscle
- Hypertrophic cardiomyopathy: thickens the heart muscle
- Restrictive cardiomyopathy: stiffens the heart muscle
- Arrhythmogenic right ventricular cardiomyopathy: replaces heart muscle tissue with fatty tissue
- Transthyretin amyloid cardiomyopathy (ATTR-CM): causes a buildup of a protein that stiffens the heart muscle
Cardiomyopathy impacts all genders and people of all ages, including children.
Family history, age, race, and other unique factors can affect the type of disease you get.
Symptoms
Cardiomyopathy impacts people differently. Some may never have signs of sickness. Others may have symptoms that grow worse as the disease causes more damage.
Signs of illness can be the same across different types of this disease. Common symptoms include:2
- Shortness of breath, especially after physical exertion
- Dizziness
- Fainting
- Chest pain
- Fatigue
- Swelling of the arms and legs
- Heart palpitations
Causes
This disease can be described as primary or secondary.3
Primary cardiomyopathy involves causes that only affect the heart muscle.
Secondary cardiomyopathy results from a condition that also affects other parts of your body.
Primary cardiomyopathy can be caused by genetic disorders, such as hypertrophic cardiomyopathy, or by disorders acquired during life, such as peripartum cardiomyopathy.3
Common causes of secondary cardiomyopathy include:3
- Autoimmune diseases such as rheumatoid arthritis
- Infections such as hepatitis C
- Endocrine diseases such as diabetes
- Neuromuscular disorders such as muscular dystrophy
- Nutritional deficits such as a niacin deficiency
- Over-exposure to toxins such as alcohol
You can also have this disease without a known cause.
Diagnosing Cardiomyopathy
A cardiomyopathy diagnosis typically occurs after you report symptoms to your healthcare provider.
Your symptoms and family history help define the types of tests you need.
Some common tests used to diagnose this disease include:4
- Blood test
- Chest X-ray
- Echocardiogram (ECG)
- Electrocardiogram (EKG)
- Treadmill stress test
- Cardiac magnetic resonance imagine (MRI)
- Cardiac computerized tomography (CT) scan
Some types of heart disease are linked to genetics. If a close family member has this illness, genetic testing may be advised.
If you have an inherited form of cardiomyopathy, genetic tests might help you assess your risk of transmitting this disease to your children.
Genetic testing can also help detect inherited forms of cardiomyopathy before they produce signs of sickness.5
Treatment
Treatment goals for people with cardiomyopathy include slowing disease progression, managing symptoms, and avoiding potential complications.
Potential treatments vary considerably depending on which type of cardiomyopathy you have, and the severity of your condition.6
ECG EQUIPMENT? VISIT THE ZOLL BOOTH AT EMERGENCY EXPO
Treating Primary Cardiomyopathy
Treatment for primary cardiomyopathy typically involves starting and keeping a healthy way of life.
This includes the following steps:6
- Eating a heart-healthy diet
- Boosting physical activity
- Reducing stress
- Limiting or avoiding alcohol
- Quitting smoking
Medicine may be prescribed to control signs of sickness. The most common types of medicines used include:7
- ACE inhibitors, angiotensin II receptor blockers (ARBs), beta blockers, and calcium channel blockers to lower blood pressure
- Beta blockers, calcium channel blockers, and Digox (digoxin) to slow an irregular heart rate
- Antiarrhythmics to prevent irregular heartbeats
- Aldosterone blockers to balance electrolytes
- Diuretics to remove excess fluid
- Anticoagulants, or blood thinners, to prevent blood clots
- Corticosteroids to reduce inflammation
Some patients with cardiomyopathy benefit from a pacemaker
This surgically implanted device monitors your heart’s rhythm.
When your heart beats too slow or too fast, a pacemaker delivers an electrical signal to restore a regular beat.
Based on your disease, you may need heart surgery to correct the damage.
Treatment for the most advanced stages of this illness may require a heart transplant.
Treating Secondary Cardiomyopathy
If you have secondary cardiomyopathy, treatment for your heart-related symptoms involves the same therapies used for primary cardiomyopathy.
Secondary cardiomyopathy may be treated with lifestyle changes, medication, an implanted medical device, and/or heart surgery.
However, treating secondary cardiomyopathy also involves addressing the underlying condition that caused your heart disease.
This is necessary to prevent further heart damage.
Treatment for secondary cardiomyopathy varies widely depending on the underlying condition.
For example, in cases of alcoholic cardiomyopathy, treatment may include the cessation of all alcohol consumption.8
Prognosis
There is no cure for cardiomyopathy.
However, a supervised treatment plan can help slow down the disease.
The right treatment can also improve your quality of life.
Your prognosis can improve if you find the illness early.
Other factors such as your age, overall health, and type of disease also affect your outlook.
Without treatment, cardiomyopathy can lead to heart failure.
This is a serious condition that can be life-threatening.
Coping With Cardiomyopathy
Living with cardiomyopathy means dealing with both physical and emotional changes.
Feeling afraid or depressed about your illness is normal.
It’s common to feel lonely or angry if your sickness limits your lifestyle.
Doing your best to take care of your physical health (e.g., following a healthy diet, exercising, getting enough sleep) can also aid your mental and emotional health.
Living a healthy lifestyle can help you maintain a sense of normalcy and routine, which makes the coping process easier.9
Realize that your feelings can affect your physical state. Getting support from others in online and in-person support groups and/or sharing your concerns with family and friends can help ease the emotional burden.
Don’t be afraid to discuss your feelings with your healthcare provider.
They may advise you to get professional help.10
References:
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Broken Heart Syndrome Is On The Rise: We Know Takotsubo Cardiomyopathy
Inflammations Of The Heart: Myocarditis, Infective Endocarditis And Pericarditis
Quickly Finding – And Treating – The Cause Of A Stroke May Prevent More: New Guidelines
Atrial Fibrillation: Symptoms To Watch Out For
Wolff-Parkinson-White Syndrome: What It Is And How To Treat It
Do You Have Episodes Of Sudden Tachycardia? You May Suffer From Wolff-Parkinson-White Syndrome (WPW)
Wolff-Parkinson-White Syndrome: Pathophysiology, Diagnosis And Treatment Of This Heart Disease




