Cardiac electrostimulation: the leadless pacemaker
As technology evolved, the leadless pacemaker was introduced in 2015; a real revolution in cardiac electrostimulation
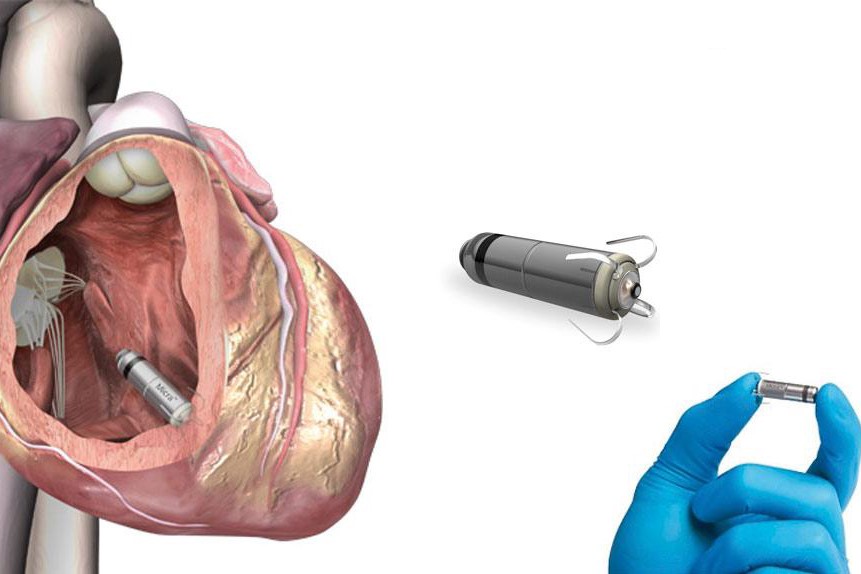
This pacemaker, without leads, is a very small implant that is implanted in the heart via a minimally invasive procedure that does not require surgery.
A pacemaker is an electronic device that monitors cardiac activity by electrically stimulating the heart if heart activity slows down.
By stimulating the heart, the pacemaker replaces the heart’s electrical system that is ‘defective’
The traditional pacemaker is made from a generator, a little larger than a 2 euro coin, and is implanted with a small surgical procedure in a subcutaneous pocket that is usually placed under the collarbone, either right or left.
It is connected to wires, the leads, which are permanently inserted into the chambers of the heart.
Their function, is to generate and transmit electrical impulses to the heart, transmitting the heart’s cardiac activity to the pacemaker.
Complications can affect up to 10% of patients.
More than 80% of complications are due to the subcutaneous pocket and the leads; the subcutaneous pocket may lead to haematoma and infection, the leads on the other hand may move, rupture or become infected.
Infection of the leads can lead to a serious infection of the heart, endocarditis, which can lead to death.
To treat the infection, the patient must undergo pacemaker explantation and lead extraction; the extraction procedure is a complex and risky operation.
Most of the complications associated with implanting a pacemaker are related to the subcutaneous pocket and the leads.
Getting rid of these two elements will eliminate pacemaker-related complications.
But, returning to the wireless pacemaker, it is an extremely small pacemaker, weighing just 2 grams and less than 3 cm long, compared to the 30 grams of the conventional pacemaker.
Its implantation is performed under local anaesthesia, is inserted via a femoral vein, and does not require any surgical cutting.
Via a small tube, the pacemaker is pushed into the heart where it anchors itself to the heart wall in order to stimulate the heart.
The implantation of such a device takes between 45 and 50 minutes, the battery life is about 10 years.
It does not require any subcutaneous pocket and has no leads that have to be inserted into the heart, so complications due to pocket and leads are also avoided.
This small, leadless pacemaker has been implanted in over 50,000 patients around the globe
It has been declared safer than the traditional pacemaker due to the reduced number of complications compared to the traditional defibrillator.
The leadless pacemaker, as it has no leads, does not require any caution on the part of the patient
After implantation of the conventional pacemaker, the patient must avoid exertion and sudden movements in order to prevent the leads from moving and risk the subcutaneous pocket wound from opening.
With the wireless pacemaker, the patient can return to normal activity as early as 2 days after surgery.
There will also be no scarring on the chest, and in this way, aesthetic and psychological impacts will also be avoided.
However, the wireless pacemaker can currently only be implanted in one chamber of the heart, namely in the right ventricle.
Therefore, not everyone can benefit from this innovative device, but only those who need the right ventricle to be stimulated.
A pacemaker is being studied that is capable of stimulating not only the right ventricle but also the rest of the heart, i.e. the left ventricle and atria.
The traditional pacemaker, over time, sees the veins and the heart encase the leads, which will be blocked inside them by real scars.
Removing them therefore becomes increasingly risky, and a probable operation to remove them would be extremely complex.
Risks associated with the implantation of a leadless pacemaker
However, the implantation of a wireless pacemaker also has risks; at the level of the femoral puncture, trauma to the vein with even major haematomas can occur, up to and including rupture of the vein.
At the level of the heart, infections may be triggered and it may happen that the device breaks free from its anchorage, floating inside the ventricle or ending up in the pulmonary artery.
During implantation, arrhythmias due to mechanical stimulation could occur.
These are possible but more than rare occurrences that only time will be able to give us sufficient numbers to draw up reliable statistics.
To date, the system is completely safe and reliable and the risks are far lower than those of a conventional pacemaker.
Therefore, if a traditional pacemaker wearer wanted to replace his pacemaker with a wireless one, he would not be able to do so.
There are pathologies that degenerate, in most cases related to ageing; these pathologies affect the heart, which is no longer able to generate the electrical impulse correctly or conduct it correctly to all parts of the heart.
This leads the heart to slow down or, in more serious cases, to stop with very serious consequences.
Therefore, the future of cardiac electrostimulation sees the wireless pacemaker as its best representative and aid in this field.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Heart Pacemaker: How Does It Work?
Paediatric Pacemaker: Functions And Peculiarities
What Is The Difference Between Pacemaker And Subcutaneous Defibrillator?
Heart: What Is Brugada Syndrome And What Are The Symptoms
Genetic Heart Disease: Brugada Syndrome
Cardiac Arrest Defeated By A Software? Brugada Syndrome Is Near To An End
Heart: Brugada Syndrome And The Risk Of Arrhythmia
Heart Disease: First Study On Brugada Syndrome In Children Under 12 From Italy
Mitral Insufficiency: What It Is And How To Treat It
Semeiotics Of The Heart: History In The Complete Cardiac Physical Examination
Electrical Cardioversion: What It Is, When It Saves A Life
Heart Murmur: What Is It And What Are The Symptoms?
Performing The Cardiovascular Objective Examination: The Guide
Branch Block: The Causes And Consequences To Take Into Account
Cardiopulmonary Resuscitation Manoeuvres: Management Of The LUCAS Chest Compressor
Supraventricular Tachycardia: Definition, Diagnosis, Treatment, And Prognosis
Identifying Tachycardias: What It Is, What It Causes And How To Intervene On A Tachycardia
Myocardial Infarction: Causes, Symptoms, Diagnosis And Treatment
Aortic Insufficiency: Causes, Symptoms, Diagnosis And Treatment Of Aortic Regurgitation
Congenital Heart Disease: What Is Aortic Bicuspidia?
Atrial Fibrillation: Definition, Causes, Symptoms, Diagnosis And Treatment
Ventricular Fibrillation Is One Of The Most Serious Cardiac Arrhythmias: Let’s Find Out About It
Atrial Flutter: Definition, Causes, Symptoms, Diagnosis And Treatment
What Is Echocolordoppler Of The Supra-Aortic Trunks (Carotids)?
What Is The Loop Recorder? Discovering Home Telemetry
Cardiac Holter, The Characteristics Of The 24-Hour Electrocardiogram
Peripheral Arteriopathy: Symptoms And Diagnosis
Endocavitary Electrophysiological Study: What Does This Examination Consist Of?
Cardiac Catheterisation, What Is This Examination?
Echo Doppler: What It Is And What It Is For
Transesophageal Echocardiogram: What Does It Consist Of?
Paediatric Echocardiogram: Definition And Use
Heart Diseases And Alarm Bells: Angina Pectoris
Fakes That Are Close To Our Hearts: Heart Disease And False Myths
Sleep Apnoea And Cardiovascular Disease: Correlation Between Sleep And Heart
Myocardiopathy: What Is It And How To Treat It?
Venous Thrombosis: From Symptoms To New Drugs
Cyanogenic Congenital Heart Disease: Transposition Of The Great Arteries
Heart Rate: What Is Bradycardia?
Consequences Of Chest Trauma: Focus On Cardiac Contusion


