Reactive arthritis: symptoms, causes and treatment
Reactive arthritis is an acute, non-purulent inflammation of the joints, which is caused by a localised infection affecting other parts of the body
This type of inflammation generally occurs 1-6 weeks after the infection, which is often sustained by microorganisms affecting the intestinal tract or genito-urinary tract.
It is a rheumatologic disease that falls into the group of seronegative spondyloarthritis, along with others, because it shares some common distinguishing features, such as positivity for the HLA-B27 antigen and negativity for rheumatoid factor.
Reactive arthritis or Reiter’s syndrome
In some cases the disease is also called Reiter’s syndrome.
In particular, it is a specific form of long-lasting reactive arthritis, which is often accompanied by:
- arthritis (inflammation of the joints);
- conjunctivitis;
- urethritis (inflammation of the urinary tract).
Inflammation of the joints usually develops in people between the ages of 18 and 40, rarely in children or the elderly.
It can occur in women and men, if it is an infection of the gastrointestinal tract, when it occurs in the genitourinary tract it is more common in men.
Every year, this discomfort affects about 1-30 individuals per 100,000 inhabitants.
Septic arthritis
It is important not to confuse reactive arthritis with septic arthritis.
The reasons are as follows:
- septic arthritis is a disease in which the pathogenic micro-organism is located directly inside the joint and can be found by analysing the synovial fluid;
- in reactive arthritis, the micro-organism causes infection of the mucous membranes of the intestinal or genitourinary tract and only then, especially in more genetically predisposed persons, can it cause non-purulent joint inflammation.
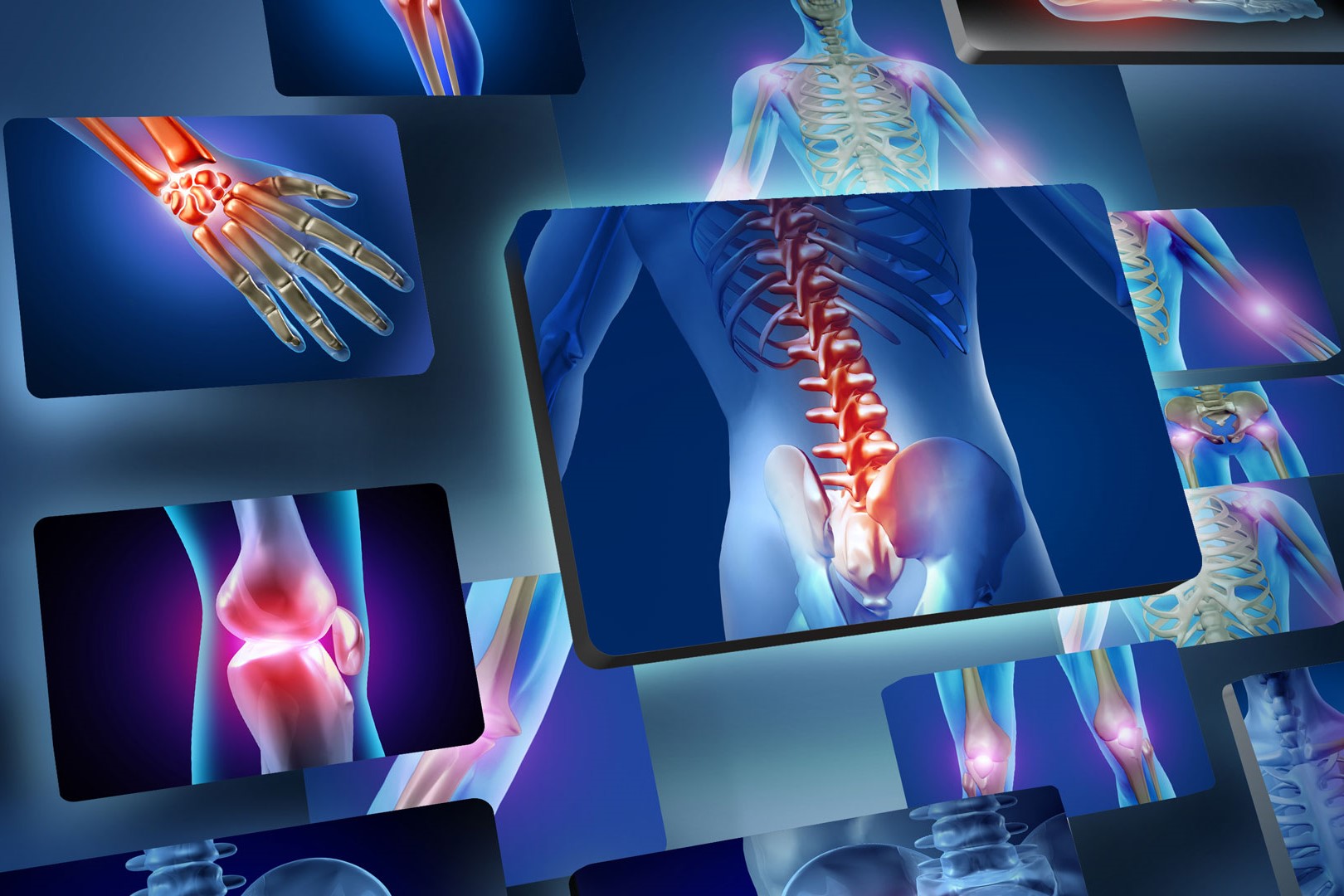
Symptoms include both articular and extra-articular manifestations
Articular manifestations generally concern the leg joints, which may present as
- swollen,
- reddened,
- stiff,
- warm,
- painful.
Extra-articular manifestations include:
- persistent tiredness
- moderate fever,
- weight loss,
- conjunctivitis
- and oral ulcers.
Causes
Joint-related illness is often caused by an infection of the gastrointestinal or genito-urinary tract.
The microbes often responsible for the infection are different and are distinguished according to the part of our body affected.
The genito-urinary tract:
- Chlamydia trachomatis;
- Ureaplasma urealyticum.
The digestive tract:
- Shigella (flexneri, sonnei);
- Yersinia (enterocolitica, pseudotuberculosis);
- Salmonella (all serotypes);
- Campylobacter (jejuni, fetus, lari).
After infection, our immune system may also consider joint and extra-articular structures as targets to fight.
So our antibodies, in addition to fighting the infection, may also target structures within our own body.
It happens only rarely and generally affects genetically more predisposed people, such as those with the HLA-B27 antigen.
Reactive arthritis, the risk factors
The main risk factor that can lead to the development of the disease is the presence of the HLA-B27 antigen.
60-85% of patients who develop reactive arthritis are HLA-B27 positive.
Human leukocyte antigens (HLA -Human leukocyte antigen) are proteins that allow the immune system to discriminate between cells in the body and foreign cells.
Each of us has a specific HLA antigen combination, present on the surface of leukocytes and other cells.
Thus, possessing the HLA-B27 antigen only predisposes to the onset of reactive arthritis and other autoimmune diseases.
The HLA-B27 antigen increases the risk of causing reactive arthritis up to 50-fold following infection of the intestinal or genito-urinary tract.
Diagnosis
To diagnose this disease, one proceeds by means of anamnesis and on the basis of the specific clinical picture of the case.
How to treat reactive arthritis
Anti-inflammatory drugs are sufficient to treat arthritis that presents in a mild form.
For more severe arthritis that is refractory to treatment with anti-inflammatory drugs, the doctor may prescribe immunosuppressive drugs (sulfasalazine, azathioprine, methotrexate). In some cases, if the severity is considerable, apremilast, a phosphodiesterase 4 inhibitor, may be recommended.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Arthrosis: What It Is And How To Treat It
Septic Arthritis: Symptoms, Causes And Treatment
Psoriatic Arthritis: How To Recognize It?
Arthrosis: What It Is And How To Treat It
Juvenile Idiopathic Arthritis: Study Of Oral Therapy With Tofacitinib By Gaslini Of Genoa
Rheumatic Diseases: Arthritis And Arthrosis, What Are The Differences?
Rheumatoid Arthritis: Symptoms, Diagnosis And Treatment
Joint Pain: Rheumatoid Arthritis Or Arthrosis?
The Barthel Index, An Indicator Of Autonomy
What Is Ankle Arthrosis? Causes, Risk Factors, Diagnosis And Treatment
Unicompartmental Prosthesis: The Answer To Gonarthrosis
Knee Arthrosis (Gonarthrosis): The Various Types Of ‘Customised’ Prosthesis
Symptoms, Diagnosis And Treatment Of Shoulder Arthrosis
Arthrosis Of The Hand: How It Occurs And What To Do
Arthritis: Definition, Diagnosis, Treatment, And Prognosis
Rheumatic Diseases: The Role Of Total Body MRI In Diagnosis
Rheumatology Tests: Arthroscopy And Other Joint Tests
Rheumatoid Arthritis: Advances In Diagnosis And Treatment
Diagnostic Tests: Arthro Magnetic Resonance Imaging (Arthro MRI)


