The Australian government: how to perform cardiopulmonary resuscitation? / VIDEO
CPR (short for cardiopulmonary resuscitation) is a first aid technique that can be used if someone is not breathing properly or if their heart has stopped
In recent weeks, an article by Queensland’s leading training organisation, First Aid Brisbane, has caused quite a stir.
It is an organisation recognised by that state of Australia, of mammoth size and great tradition and authority, which has expressed a position that we can describe as ‘non Ilcor’, so to speak.
We therefore went looking for that of the Australian Ministry of Health, which we quote in full.
With one caveat: the two positions are not mutually exclusive. Australia, in fact, is a federal state in which the individual member states enjoy an autonomy, in some areas, that is unparalleled in the world.
RESCUE RADIO IN THE WORLD? VISIT THE EMS RADIO BOOTH AT EMERGENCY EXPO
CPR, what the government of Australia says
CPR (short for cardiopulmonary resuscitation) is a first aid technique that can be used if someone is not breathing properly or if their heart has stopped.
- CPR is a skill that everyone can learn — you don’t need to be a health professional to do it.
- Try to stay calm if you need to do CPR.
- Performing CPR may save a person’s life.
- If you know CPR, you might save the life of a family member or friend.
Start CPR as soon as possible
CPR involves chest compressions and mouth-to-mouth (rescue breaths) that help circulate blood and oxygen in the body. This can help keep the brain and vital organs alive.
You should start CPR if a person:
- is unconscious
- is not responding to you
- is not breathing, or is breathing abnormally
How to perform CPR — adults
Watch this video from Royal Life Saving Australia about how to perform CPR on an adult, or read the DRS ABCD action plan and step-by-step instructions below.
Follow these steps before starting CPR. (Use the phrase “doctor’s ABCD” — DRS ABCD — to help you remember the first letter of each step.)
CPR – ADULTS: DRSABCD ACTION PLAN
Letter Representing What to do
D Danger Ensure that the patient and everyone in the area is safe. Do not put yourself or others at risk. Remove the danger or the patient.
R Response Look for a response from the patient — loudly ask their name, squeeze their shoulder.
S Send for help If there is no response, phone triple zero (000) or ask another person to call. Do not leave the patient.
A Airway Check their mouth and throat is clear. Remove any obvious blockages in the mouth or nose, such as vomit, blood, food or loose teeth, then gently tilt their head back and lift their chin.
B Breathing Check if the person is breathing abnormally or not breathing at all after 10 seconds. If they are breathing normally, place them in the recovery position and stay with them.
C CPR If they are still not breathing normally, start CPR. Chest compressions are the most important part of CPR. Start chest compressions as soon as possible after calling for help.
D Defibrillation Attach an Automated External Defibrillator (AED) to the patient if one is available and there is someone else who is able to bring it. Do not get one yourself if that would mean leaving the patient alone.
TRAINING: VISIT THE BOOTH OF DMC DINAS MEDICAL CONSULTANTS IN EMERGENCY EXPO
Carry out chest compressions:
- Place the patient on their back and kneel beside them.
- Place the heel of your hand on the lower half of the breastbone, in the centre of the person’s chest. Place your other hand on top of the first hand and interlock your fingers.
- Position yourself above the patient’s chest.
- Using your body weight (not just your arms) and keeping your arms straight, press straight down on their chest by one third of the chest depth.
- Release the pressure. Pressing down and releasing is 1 compression.
Give mouth-to-mouth:
- Open the person’s airway by placing one hand on the forehead or top of the head and your other hand under the chin to tilt the head back.
- Pinch the soft part of the nose closed with your index finger and thumb.
- Open the person’s mouth with your thumb and fingers.
- Take a breath and place your lips over the patient’s mouth, ensuring a good seal.
- Blow steadily into their mouth for about 1 second, watching for the chest to rise.
- Following the breath, look at the patient’s chest and watch for the chest to fall. Listen and feel for signs that air is being expelled. Maintain the head tilt and chin lift position.
- If their chest does not rise, check the mouth again and remove any obstructions. Make sure the head is tilted and chin lifted to open the airway. Check that yours and the patient’s mouth are sealed together and the nose is closed so that air cannot easily escape. Take another breath and repeat.
Give 30 compressions followed by 2 breaths, known as “30:2”. Aim for 5 sets of 30:2 in about 2 minutes (if only doing compressions about 100 – 120 compressions per minute).
Keep going with 30 compressions then 2 breaths until:
- the person recovers — they start moving, breathing normally, coughing or talking — then put them in the recovery position; or
- it is impossible for you to continue because you are exhausted; or
- the ambulance arrives and a paramedic takes over or tells you to stop
Doing CPR is very tiring so if possible, with minimal interruption, swap between doing mouth-to-mouth and compressions so you can keep going with effective compressions.
If you can’t give breaths, doing compressions only without stopping may still save a life.
How to perform CPR — children over 1 year
Use these instructions only if the child’s chest is too small for you to use both hands to do chest compressions. Otherwise, use the instructions for adult CPR above.
Watch this video from Royal Life Saving Australia about how to perform CPR on a child, or read the DRS ABCD action plan and step-by-step instructions below.
Follow these steps before starting CPR. (Use the phrase “doctor’s ABCD” — DRS ABCD — to help you remember the first letter of each step.)
CHILDREN OVER 1 YEAR, CPR: DRSABCD ACTION PLAN
Letter Representing What to do
D Danger Ensure that the patient and everyone in the area is safe. Do not put yourself or others at risk. Remove the danger or the patient.
R Response Look for a response from the patient — loudly ask their name, squeeze their shoulder.
S Send for help If there is no response, phone triple zero (000) or ask another person to call. Do not leave the patient.
A Airway Check their mouth and throat is clear. Remove any obvious blockages in the mouth or nose, such as vomit, blood, food or loose teeth, then gently tilt their head back and lift their chin.
B Breathing Check if the person is breathing abnormally or not breathing at all after 10 seconds. If they are breathing normally, place them in the recovery position and stay with them.
C CPR If they are still not breathing normally, start CPR. Chest compressions are the most important part of CPR. Start chest compressions as soon as possible after calling for help.
D Defibrillation Attach an Automated External Defibrillator (AED) to the patient if one is available and there is someone else who is able to bring it. Do not get one yourself if that would mean leaving the patient alone.
To carry out chest compressions on a child:
- Place the child on their back and kneel beside them.
- Place the heel of one hand on the lower half of breastbone, in the centre of the child’s chest (the size of the child will determine if you do CPR with 1 hand or 2 hands).
- Position yourself above the child’s chest.
- Keeping your arm or arms straight, press straight down on their chest by one third of the chest depth.
- Release the pressure. Pressing down and releasing is 1 compression.
To give mouth-to-mouth to a child:
- Open the child’s airway by placing one hand on the forehead or top of the head and your other hand under the chin to tilt the head back.
- Pinch the soft part of the nose closed with your index finger and thumb.
- Open the child’s mouth with your thumb and fingers.
- Take a breath and place your lips over the child’s mouth, ensuring a good seal.
- Blow steadily into their mouth for about 1 second, watching for the chest to rise.
- Following the breath, look at the child’s chest and watch for the chest to fall. Listen and feel for signs that air is being expelled. Maintain the head tilt and chin lift position.
- If their chest does not rise, check the mouth again and remove any obstructions. Make sure the head is tilted and chin lifted to open the airway. Check that yours and the child’s mouth are sealed together, and the nose is closed so that air cannot easily escape. Take another breath and repeat.
Give 30 compressions followed by 2 breaths, known as “30:2”. Aim for 5 sets of 30:2 in about 2 minutes (if only doing compressions about 100 – 120 compressions per minute).
Keep going with 30 compressions then 2 breaths until:
- the child recovers – they start moving, breathing normally, coughing or talking — then put them in the recovery position; or
- it is impossible for you to continue because you are exhausted; or
- the ambulance arrives and a paramedic takes over or tells you to stop
Doing CPR is very tiring so if possible, with minimal interruption, swap between doing mouth-to-mouth and compressions so you can keep going with effective compressions.
If you can’t give breaths, doing compressions only without stopping may still save a life.
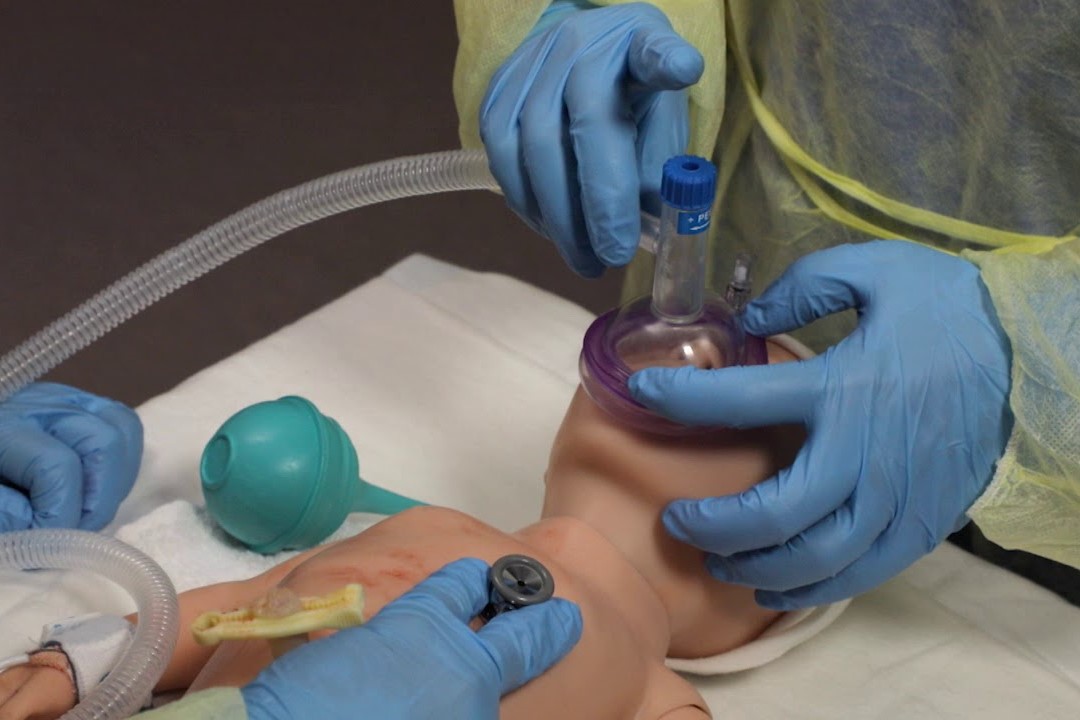
How to perform CPR — babies under 1 year
Watch this video from Royal Life Saving Australia about how to perform CPR on a baby, or read the DRS ABC action plan and step-by-step instructions below.
Follow these life support steps before starting. (Use the phrase “doctor’s ABC” — DRS ABC — to help you remember the first letter of each step.)
BEBIES UNDER 1 YEAR, CPR: DRSABCD ACTION PLAN
| D | Danger | Ensure that the baby/infant and all people in the area are safe. Remove the danger or the baby/infant. |
| R | Response | Look for a response from the baby/infant — check for a response to a loud voice, or gently squeeze their shoulders. Do not shake the baby/infant. |
| S | Send for help | If there is no response, phone triple zero (000) or ask another person to call. Do not leave the patient. |
| A | Airway | Gently lift the baby’s chin to a neutral position (with the head and neck in line, not tilted). Check in the mouth for any blockages, such as vomit, an object or loose teeth, and clear it out with your finger. |
| B | Breathing | Check if the baby/infant is breathing abnormally or not breathing at all after 10 seconds. If they are breathing normally, place them in the recovery position and stay with them. |
| C | CPR | If they are still not breathing normally, start CPR. Chest compressions are the most important part of CPR. Start chest compressions as soon as possible after calling for help… |
To carry out chest compressions on a baby:
- Lie the baby/infant on their back.
- Place 2 fingers on the lower half of the breastbone in the middle of the chest and press down by one-third of the depth of the chest (you may need to use one hand to do CPR depending on the size of the infant).
- Release the pressure. Pressing down and releasing is 1 compression.
To give mouth-to-mouth to a baby:
- Tilt the baby/infant’s head back very slightly.
- Lift the baby/infant’s chin up, be careful not to rest your hands on their throat because this will stop the air getting to their lungs from the mouth-to-mouth.
- Take a breath and cover the baby/infant’s mouth and nose with your mouth, ensuring a good seal.
- Blow steadily for about 1 second, watching for the chest to rise.
- Following the breath, look at the baby/infant’s chest and watch for the chest to fall. Listen and feel for signs that air is being expelled.
- If their chest does not rise, check their mouth and nose again and remove any obstructions. Make sure their head is in a neutral position to open the airway and that there is a tight seal around the mouth and nose with no air escaping. Take another breath and repeat.
Give 30 compressions followed by 2 breaths, known as “30:2”. Aim for 5 sets of 30:2 in about 2 minutes (if only doing compressions about 100 – 120 compressions per minute).
Keep going with 30 compressions to 2 breaths until:
- the baby/infant recovers — they start moving, breathing normally, coughing, crying or responding — then put them in the recovery position (see above); or
- it is impossible for you to continue because you are exhausted; or
- the ambulance arrives and a paramedic takes over or tells you to stop
If you can’t give breaths, doing compressions only without stopping may still save a life
Using an automated external defibrillator (AED)
Using an AED can also save someone’s life. You do not need to be trained to use an AED since the AED will guide you with voice prompts on how to use it safely.
- Attach the AED and follow the prompts.
- Continue CPR until the AED is turned on and the pads attached.
- The AED pads should be placed as instructed and should not be touching each other.
- Make sure no-one touches the person while the shock is being delivered.
- You can use a standard adult AED and pads on children over 8 years old. Children younger than 8 should ideally have paediatric pads and an AED with a paediatric capability. If these aren’t available, then use the adult AED.
- Do not use an AED on children under 1 year of age.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Let’s Talk About Ventilation: What Are The Differences Between NIV, CPAP And BIBAP?
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Drowning Resuscitation For Surfers
First Aid: When And How To Perform The Heimlich Maneuver / VIDEO
Mild, Moderate, Severe Mitral Valve Insufficiency: Symptoms, Diagnosis And Treatment
First Aid, The Five Fears Of CPR Response
Perform First Aid On A Toddler: What Differences With The Adult?
Heimlich Maneuver: Find Out What It Is And How To Do It
Respiratory Arrest: How Should It Be Addressed? An Overview
How To Manage A Prehospital Burn?
Irritant Gas Inhalation Injury: Symptoms, Diagnosis And Patient Care
Chest Trauma: Clinical Aspects, Therapy, Airway And Ventilatory Assistance
Internal Haemorrhage: Definition, Causes, Symptoms, Diagnosis, Severity, Treatment
Introduction To Advanced First Aid Training
First Aid Guide For The Heimlich Manoeuvre
Temporal And Spatial Disorientation: What It Means And What Pathologies It Is Associated With
Concussion: What It Is, What To Do, Consequences, Recovery Time
Emergency Rescue: Comparative Strategies To Exclude Pulmonary Embolism
Pneumothorax And Pneumomediastinum: Rescuing The Patient With Pulmonary Barotrauma
Barotrauma Of The Ear And Nose: What It Is And How To Diagnose It
Clinical Review: Acute Respiratory Distress Syndrome
Stress And Distress During Pregnancy: How To Protect Both Mother And Child
Respiratory Distress: What Are The Signs Of Respiratory Distress In Newborns?
Sepsis: Survey Reveals The Common Killer Most Australians Have Never Heard Of
Sepsis, Why An Infection Is A Danger And A Threat To The Heart
Respiratory Distress Syndrome (ARDS): Therapy, Mechanical Ventilation, Monitoring


