Mild, moderate, severe mitral valve insufficiency: symptoms, diagnosis and treatment
Mitral insufficiency is a condition characterised by a defect in the closure of the mitral valve (also called ‘mitral valve’), which causes part of the blood pumped from the left ventricle to flow back into the left atrium instead of remaining in the ventricle and then going into the aorta, causing fatigue and respiratory disorders
Synonyms for mitral insufficiency are: mitral insufficiency, mitral incontinence, mitral incontinence, mitral valve incontinence, mitral valve insufficiency, mitral valve insufficiency, mitral valve insufficiency, mitral regurgitation and left atrium-ventricle insufficiency.
What is mitral insufficiency?
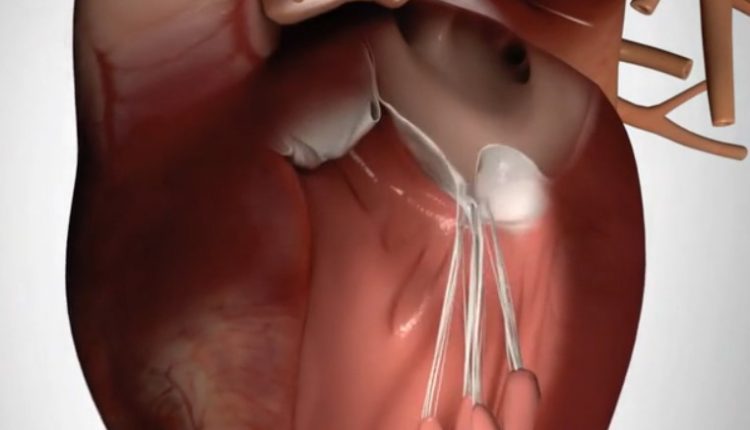
Under normal conditions, the mitral valve is formed by two thin movable leaflets anchored by cords of tendon to two muscles (the papillary muscles) which, by contracting together with the left ventricle where they are located, prevent the mitral leaflets from flaring (prolapsing) into the left atrium: the edges of the leaflets separate when the valve opens, allowing blood to pass from the left atrium into the left ventricle, and come together again when the valve closes, preventing blood from flowing back.
In a healthy heart, the mitral valve hermetically separates the left atrium from the left ventricle.
When, however, this valve does not close properly, this results in what is known as mitral insufficiency, a condition in which some of the blood that should be pushed from the left ventricle into the aorta instead flows back into the atrium.
Regardless of the cause, this situation can lead to fatigue of the heart, with dilation of the left ventricle. The consequences can be heart failure and heart rhythm abnormalities, such as atrial fibrillation, but also endocarditis.
What are the causes of mitral insufficiency?
There are several conditions that lead to mitral valve insufficiency. Depending on the causes, mitral insufficiency can be primary or secondary:
- primary mitral insufficiency: there are anatomical changes in the mitral valve apparatus such as alterations in the valve leaflets caused, for example, by endocarditis or rheumatic disease, stretching or rupture of the chordae tendineae resulting in prolapse of the valve leaflets, calcifications of the mitral ring, traumatic rupture of a papillary muscle.
- Secondary mitral insufficiency: the valve is anatomically normal and the closure defect is caused by a severe impairment of the contractile function of the left ventricle (heart failure), which is often secondary to ischaemic heart disease.
What are the symptoms and signs of mitral insufficiency?
The symptoms of mitral insufficiency depend on the severity and speed of onset and progression; they may include shortness of breath (especially during physical activity or when lying down), easy fatigability, (especially at night or when lying down), palpitations, and swelling of the feet and ankles.
How to prevent mitral insufficiency?
To minimise the risk of mitral insufficiency, it is important to appropriately treat conditions that could trigger it, such as throat infections that can lead to rheumatic disease (an autoimmune syndrome that can be triggered by streptococcal infections).
Diagnosis of mitral insufficiency
In the presence of symptoms suggestive of mitral insufficiency, the doctor carries out a thorough objective examination in which, in particular, he listens to the patient’s heart: this may typically reveal the presence of a heart murmur.
The next diagnostic step is to perform various diagnostic tests, including:
- Blood pressure measurement: Using a sphygmomanometer, the doctor measures the patient’s blood pressure, which should preferably be within the range of 130 (maximum) and 90 (minimum).
- Electrocardiogram (ECG): records the electrical activity of the heart. It can show multiple alterations, in particular signs of left atrial dilatation, signs of hypertrophy and overload (‘overwork’) of the left ventricle, arrhythmias such as atrial fibrillation.
- Chest X-ray (chest X-ray): signs of left atrial and ventricular dilatation and pulmonary congestion may be present.
- Transthoracic echocardiogram with colordoppler: ultrasound of the heart is an imaging test that visualises the structures of the heart and the functioning of its moving parts. The device sends an ultrasound beam to the thorax, through a probe resting on its surface, and reprocesses the reflected ultrasounds that return to the same probe after interacting in different ways with the various components of the heart structure (myocardium, valves, cavities). Ultrasound of the heart, combined with an investigation with a colordoppler, is a fundamental examination because it makes it possible to assess the mechanism and extent of mitral insufficiency as well as the size of the atrium and left ventricle, the contractile function of the latter and the presence of pulmonary hypertension. The colordoppler clearly identifies blood that, due to the valve insufficiency, flows back into the atrium instead of remaining confined in the atrium. Real-time images can also be collected during a stress test (stress echo): the performance of a stress echo is indicated when there is a discrepancy between the severity of symptoms and the extent of mitral insufficiency at rest.
- Transesophageal echocardiogram: the probe is in this case introduced through the mouth and pushed forward until it reaches the oesophagus. It allows better visualisation of the valves and paravalvular structures. It is indicated when the transthoracic echocardiogram is inconclusive and, in particular, when endocarditis is suspected.
- Exercise test: the examination consists of recording an electrocardiogram while the patient performs physical exercise, usually walking on a treadmill or pedalling on an exercise bike. It can be done to confirm the absence of symptoms in the presence of severe mitral insufficiency and to assess exercise tolerance.
- Coronarography: this is the examination that makes it possible to visualise the coronary arteries by injecting radiopaque contrast medium into them. The examination is performed in a special radiology room, in which all necessary sterility measures are observed. The injection of contrast into the coronary arteries involves the selective catheterisation of an artery and the advancement of a catheter to the origin of the explored vessels. Coronarography is indicated when mitral insufficiency is suspected to be secondary to ischaemic heart disease.
- MRI heart with mdc: produces detailed images of the structure of the heart and blood vessels by recording a signal emitted by cells subjected to an intense magnetic field. It makes it possible to assess the morphology of heart structures, cardiac function and any alterations in wall motion (hypokinesias or akinesias). The intravenous administration of contrast medium also makes it possible to distinguish whether any alterations in wall motion are due to fibrosis (=absence of myocardial viability) or ischaemia. This investigation therefore finds its elective application in mitral insufficiency secondary to ischaemic heart disease, as a ‘guide’ to possible myocardial revascularisation interventions.
Treatments of mitral insufficiency
The treatment of mitral insufficiency depends on various factors:
- on the age of the patient
- the severity of the valve defect (mild, moderate or severe insufficiency);
- on the accompanying symptoms and signs;
- the presence or absence of signs of left ventricular dysfunction;
- the association with other pathologies (e.g. arterial hypertension or previous heart attack);
- whether it is primary or secondary.
Treatment of primary mitral insufficiency
If the mitral insufficiency is primary and mild or mild/moderate and asymptomatic, there is generally no intervention and it is limited to periodic clinical and echocardiographic checks. In some cases, sporting activity may be limited by the pathology.
In the presence of severe primary chronic mitral insufficiency, surgery to repair (preferably) or replace the mitral valve is indicated.
Secondary mitral insufficiency therapy
The therapy of secondary chronic mitral insufficiency consists of treating the heart failure that is the cause and can use various types of drugs and instruments:
- beta-blockers;
- ACE-inhibitors/sartan
- anti-aldosteronics;
- digoxin;
- diuretics in the event of fluid accumulation;
- implantation of biventricular pacemakers (PM) and/or automatic defribrillators (ICDs).
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Mitral Valve Prolapse: Symptoms, Causes And Complications
Defibrillator: What It Is, How It Works, Price, Voltage, Manual And External
The Patient’s ECG: How To Read An Electrocardiogram In A Simple Way
Signs And Symptoms Of Sudden Cardiac Arrest: How To Tell If Someone Needs CPR
Mitral Valve Diseases, Causes And Symptoms
Heart Patients And Heat: Cardiologist’s Advice For A Safe Summer
Mitral Valve Diseases, The Advantages Of Mitral Valve Repair Surgery
COVID-19 Infections Increase Risk Of Heart Conditions Up To A Year Later
Inflammations Of The Heart: Myocarditis, Infective Endocarditis And Pericarditis
Quickly Finding – And Treating – The Cause Of A Stroke May Prevent More: New Guidelines
Atrial Fibrillation: Symptoms To Watch Out For
Wolff-Parkinson-White Syndrome: What It Is And How To Treat It
Do You Have Episodes Of Sudden Tachycardia? You May Suffer From Wolff-Parkinson-White Syndrome (WPW)
Transient Tachypnoea Of The Newborn: Overview Of Neonatal Wet Lung Syndrome
Tachycardia: Is There A Risk Of Arrhythmia? What Differences Exist Between The Two?



