Fires, smoke inhalation and burns: symptoms, signs, rule of nine
Fires are an important cause of injury, death and economic damage. Smoke inhalation-induced damage leads to a dramatic worsening of mortality in burn patients: in these cases, smoke inhalation damage is added to burn damage, with often fatal consequences
Symptoms, signs and diagnosis in fire victims
The increased morbidity and mortality associated with inhalation injuries in burn patients necessitates their prompt recognition and treatment.
Rapid clinical test, fibreoptic bronchoscopy, chest X-ray, haemogasanalysis, ECG and haemodynamic monitoring are the key steps in the diagnostic procedure.
The assiduous monitoring of the patient by these methods allows timely and appropriate action to be taken if necessary.
Some important details may be useful in the assessment and initial treatment of fire victims who have inhaled smoke.
A positive history of exposure to an enclosed, highly smoky environment should lead one to suspect inhalation injury, even in the absence of clear clinical signs.
A state of unconsciousness should make asphyxia and/or carbon monoxide (CO) and cyanide (RCN) poisoning more likely.
The classic sign of a cherry-red skin colour in cases of CO poisoning is not reliable on its own.
FIRST AID: VISIT THE DMC DINAS MEDICAL CONSULTANTS BOOTH AT EMERGENCY EXPO
Oximetry is an important test for the diagnosis of CO intoxication, however, low Hbco levels do not exclude the possibility of significant lung damage in the intermediate and late stages after a burn.
Pulse oximetry is the fifth vital parameter in monitoring acute patients, however, SpO2 does not accurately reflect Hbo concentrations in patients with CO poisoning because oxyhaemoglobin and Hbco have a similar light absorption spectrum, therefore, SpO2 values will be falsely elevated in patients with CO poisoning.
Pulse oximetry proves useful only in burn patients with near-normal Hbco values.
Facial burns, burnt vibrissae, buccal and laryngeal oedema, charred debris in the airways and sputum suggest inhalation injury, but their absence does not rule it out.
The presence of charred particles in sputum, which is also considered a very sensitive sign of smoke inhalation, may not be detected for 8-24 hours, and only occurs in about 40 % of subjects with lung injury.
Laryngeal stridor, hoarseness, slurred speech and thoracic retractions suggest the presence of an upper airway lesion and the need for a thorough evaluation of this.
Laryngoscopy and fibreoptic bronchoscopy are very useful for both the search of upper airway lesions and the removal of excess saliva and debris that may be present.
The appearance of coughing, dyspnoea, tachypnoea, cyanosis, hissing, wheezing or rhonchi indicate more serious inhalation injuries.
An electrocardiogram (ECG) often shows tachycardia and may also show signs of ischaemic heart disease.
SETTING UP SPECIAL VEHICLES FOR FIRE BRIGADES: DISCOVER THE PROSPEED BOOTH AT THE EMERGENCY EXPO
A chest X-ray test often shows no signs of inhalation injury
A scintigraphic study performed after intravenous injection of xenon-133 is indicative of small airway injury if complete elimination of the isotope does not occur within 90 seconds.
Unfortunately, it is not practical to perform this test in the early phase of treatment.
Spirometry has proven useful for detecting small airway and upper airway lesions.
Both maximum expiratory flow and forced expiratory rate at 50% of forced vital capacity are markedly reduced.
The applicability of this method, however, is limited to those patients who can carry out the examiner’s commands and make an adequate respiratory effort.
Arterial blood gas analysis (ABG) is very useful for assessing the severity and progression of lung injury.
A reduction in PaO2 and an increase in P(A-a)O2 (greater than 300), or a reduction in the PaO2/FiO2 ratio (less than 350), are practical and sensitive indicators of impaired respiratory function.
A respiratory alkalosis is common in the period immediately following a burn and often continues with the hypermetabolic phase.
A respiratory acidosis is indicative of respiratory failure and is usually associated with severe hypoxaemia.
Asphyxiation, elevated Hbco levels (above 40), HCN poisoning and low cardiac output are all factors potentially leading to severe metabolic acidosis.
Electrocardiogram (ECG) and haemodynamic monitoring are essential in patients with third-degree burns extending over more than 10 per cent of the body surface, whether or not associated with inhalation injury.
In extensive burns, particularly those complicated by inhalation injury, pulmonary arterial pressure, cardiac output and other haemodynamic variables can be monitored to optimise fluid infusion during resuscitation, avoiding hypotension, renal failure and fluid overload.
SPECIAL VEHICLES FOR FIREFIGHTERS: VISIT THE ALLISON BOOTH AT EMERGENCY EXPO
Fire burns, the rule of nine
The assessment of skin injuries is carried out by means of physical examination, body weight testing (to follow the water balance) and determination of the extent of the burnt body surface.
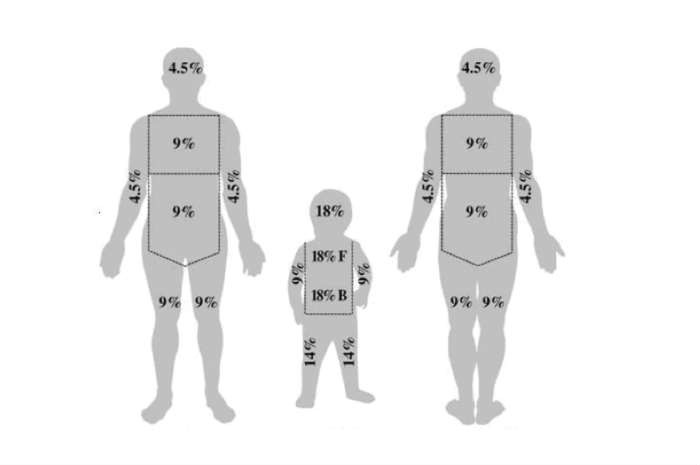
The latter can be roughly calculated, applying the so-called rule of nine, after determining the degree of involvement of the head, front and back of the trunk and limbs.
In the rule of nine, in the adult, each anatomical area represents approximately 4.5% or 9% or 18% of the total body surface.
The depth of the burn is assessed on the basis of its clinical appearance, always keeping this brief information in mind:
- first degree burn: Burn to the epithelium, manifesting as erythema and pain;
- second degree burn: Burn of the epidermis and dermis, manifesting with erythema, blistering and pain
- third-degree burn: Burn that destroys the skin down to the hypodermis or within the hypodermis and is manifested by a pale or greyish-brownish discolouration of the affected surface, which is not painful, due to the complete destruction of all sensory organs in the skin.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Calculating The Surface Area Of A Burn: The Rule Of 9 In Infants, Children And Adults
First Aid, Identifyng A Severe Burn
Chemical Burns: First Aid Treatment And Prevention Tips
Electrical Burn: First Aid Treatment And Prevention Tips
6 Facts About Burn Care That Trauma Nurses Should Know
Blast Injuries: How To Intervene On The Patient’s Trauma
What Should Be In A Paediatric First Aid Kit
Compensated, Decompensated And Irreversible Shock: What They Are And What They Determine
Burns, First Aid: How To Intervene, What To Do
First Aid, Treatment For Burns And Scalds
Wound Infections: What Causes Them, What Diseases They Are Associated With
Patrick Hardison, The Story Of A Transplanted Face On A Firefighter With Burns
Electric Shock First Aid And Treatment
Electrical Injuries: Electrocution Injuries
Emergency Burn Treatment: Rescuing A Burn Patient
Disaster Psychology: Meaning, Areas, Applications, Training
Medicine Of Major Emergencies And Disasters: Strategies, Logistics, Tools, Triage
Fires, Smoke Inhalation And Burns: Stages, Causes, Flash Over, Severity
Earthquake And Loss Of Control: Psychologist Explains The Psychological Risks Of An Earthquake
Civil Protection Mobile Column In Italy: What It Is And When It Is Activated
New York, Mount Sinai Researchers Publish Study On Liver Disease In World Trade Center Rescuers
PTSD: First responders find themselves into Daniel artworks
Firefighters, UK Study Confirms: Contaminants Increase The Likelihood Of Getting Cancer Fourfold
Civil Protection: What To Do During A Flood Or If A Inundation Is Imminent
Earthquake: The Difference Between Magnitude And Intensity
Earthquakes: The Difference Between The Richter Scale And The Mercalli Scale
Difference Between Earthquake, Aftershock, Foreshock And Mainshock
Major Emergencies And Panic Management: What To Do And What NOT To Do During And After An Earthquake
Earthquakes And Natural Disasters: What Do We Mean When We Talk About The ‘Triangle Of Life’?
Earthquake Bag, The Essential Emergency Kit In Case Of Disasters: VIDEO
Disaster Emergency Kit: how to realize it
Earthquake Bag : What To Include In Your Grab & Go Emergency Kit
How Unprepared Are You For An Earthquake?
Emergency preparedness for our pets
Difference Between Wave And Shaking Earthquake. Which Does More Damage?