Aortic valve surgery: an overview
Aortic valve surgery is performed by cardiac surgeons to treat bicuspid valve, other congenital aortic valve disorders, aortic valve stenosis, and aortic valve regurgitation
What is the aortic valve?
The heart is made up of four valves: mitral, tricuspid, aortic, and pulmonary.
The aortic valve sits between the left ventricle (the heart’s lower pumping chamber) and the aorta, which is the largest artery in the body.
The valves maintain unidirectional blood flow through the heart.
What is aortic valve disease?
Aortic valve disease occurs when the aortic valve doesn’t work properly.
It can be caused by:
- Aortic valve stenosis: These stiff, fused, thickened, inflexible leaflets of the valve lead to narrowing of the aortic valve, restricting blood flow. Aortic valve stenosis progresses when calcium is deposited on the valve leaflets, further limiting their mobility. Stenosis can occur in patients with a tricuspid (3 leaflet) or bicuspid (2 leaflet) aortic valve.
- Aortic valve regurgitation (also called valve insufficiency, incompetence, or “leaky valve”): These valve flaps don’t close completely. Regurgitation causes blood ejected from the heart to immediately flow back into it once the heart stops squeezing and relaxes. Regurgitation can occur due to floppy leaflets (prolapse), abnormal congenitally deformed valves (bicuspid or unicuspid), an infection of the valve (endocarditis), the inability of the leaflets to close tightly due to dilation of the aorta ( aneurysm), holes in the leaflets or rheumatic disease of the valve.
What are the causes of aortic valve disease?
The aortic valve may be abnormal at birth (typically a congenital bicuspid aortic valve) or become diseased over time, usually in older patients (acquired valve disease).
Congenital disease of the aortic valve
Patients with a bicuspid aortic valve are born with it and are present in about 1-2% of the population.
Instead of the normal three leaflets or cusps, the bicuspid aortic valve has only two.
Without the third leaflet, the valve opening may not close fully and leak (regurgitation) or may not open fully and narrow (stenosis) or leak.
In many cases, the bicuspid aortic valve can function normally for several years without requiring treatment.
About 25% of patients with a bicuspid aortic valve may have an enlargement of the aorta over the valve.
If it is severely distended, the aorta is known as aneurysmal.
Acquired diseases of the aortic valve
In acquired pathologies of the aortic valve, changes in the structure of the valve occur.
Acquired aortic valve conditions include:
- Infective endocarditis is a bacterial infection of the valve, caused when bacteria enter the bloodstream from the site of a remote infection and attach themselves to the surface of the heart valves. Teeth cleaning or even a minor infection, such as a tooth abscess, can cause severe bacterial endocarditis of the aortic valve.
- Rheumatic fever is usually caused by a bacterial infection of the throat, such as strep throat. In rheumatic fever, the valve itself is not infected, but antibodies developed by the body to fight the infection react with the heart valves, causing the aortic valve leaflets to stiffen and fuse together.
- Aortic valve degeneration due to wear and tear is another cause of acquired aortic valve disease. In many patients, the leaflets of the aortic valve degenerate and calcify over time. This phenomenon most often causes aortic stenosis, but it can also cause aortic regurgitation. This is the most common cause of aortic stenosis in people over the age of 65.
- Other causes of aortic valve disease are: rheumatoid arthritis, chronic inflammatory diseases, lupus, syphilis, high blood pressure, aortic aneurysms, connective tissue diseases, and less commonly, cancers, certain types of drugs, and radiation for cancers or lymphomas.
What are the symptoms of aortic valve disease?
Many patients with aortic valve disease are asymptomatic (have no symptoms), even when the stenosis (narrowing) or regurgitation (leakage) is severe.
Initial symptoms of aortic valve disease usually include:
- tiredness
- Easy tiredness
- Energy loss
- Swelling in the ankles
- Palpitations (extra or skipped heart beats)
More advanced symptoms can include
- Shortness of breath
- chest pain
- Dizziness or loss of consciousness
How is aortic valve disease diagnosed?
Diagnosing aortic valve disease is made after your doctor reviews your symptoms, does a physical exam and listens for a murmur, and evaluates the results of diagnostic tests.
During the physical exam, using a stethoscope, the doctor may hear a murmur, which represents turbulent blood flow through an abnormal valve.
The diagnosis of aortic valve disease is confirmed by a specialized ultrasound of the heart, called an echocardiogram.
The echocardiogram allows the doctor to visualize the heart valves and to determine the severity and possible cause of the aortic valve disease.
In most patients, a standard transthoracic echocardiogram (in which a gel-filled probe is placed on the skin of the chest to transmit images) is sufficient to visualize the valve.
The exam may be combined with exercise or intravenous infusion of medication to allow the doctor to see the degree of stricture more clearly.
Sometimes a transesophageal echocardiogram (TEE – where a tube is passed through the mouth into the esophagus) is needed to view the valve more closely.
TEE is an outpatient procedure.
How is aortic valve disease treated?
If there are no symptoms or damage to the heart, the valve should be protected from further damage by following precautions to reduce the risk of infective endocarditis, and medications may be required.
Also, you may need surgery to treat the condition if you have symptoms, evidence of heart damage, or heart failure.
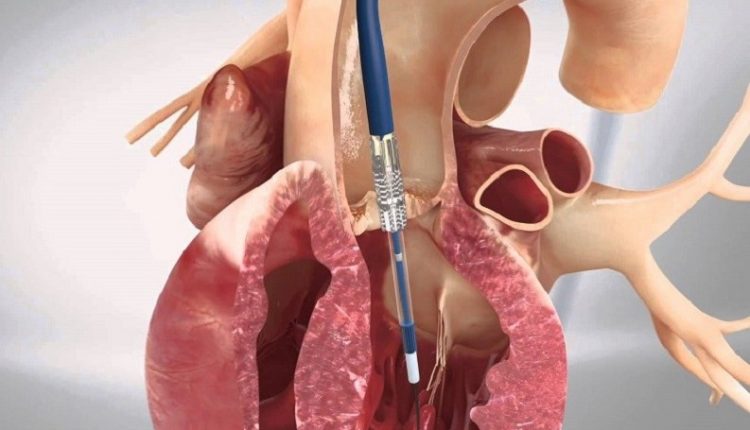
Aortic valve surgery
There are two types of aortic valve surgery: aortic valve repair and aortic valve replacement.
During aortic valve surgery, including aortic surgery, the aortic valve may be repaired or replaced.
Diagnostic test results, the structure of the heart, age, the presence of other medical conditions, and other factors will be taken into consideration to determine whether aortic valve repair or replacement is the best treatment approach for the patient.
Aortic valve surgery can be performed with traditional valve surgery or with minimally invasive approaches.
Traditional aortic valve surgery
During traditional aortic valve surgery, the surgeon makes a 6-8 inch incision in the center of the breastbone and divides part or all of the breastbone to provide direct access to the heart.
The surgeon repairs or replaces the abnormal heart valve or valves.
Minimally invasive surgery of the aortic valve
Minimally invasive aortic valve surgery is a type of aortic valve repair surgery done through smaller incisions, 2 to 4 inches, without opening up the entire chest.
It is usually done with a “J” incision and leaves the chest stable.
Minimally invasive surgery reduces blood loss, trauma, length of hospital stay, and can speed recovery.
Most patients who need isolated aortic valve surgery are candidates for minimally invasive aortic valve surgery, but your surgeon will review your diagnostic tests and determine if you are a candidate for this type of surgery.
Aortic valve repair
Although the aortic valve is usually replaced, aortic valve repair may be an option.
Bicuspid aortic valve repair
A bicuspid aortic valve can be repaired by reshaping the leaflets of the aortic valve so that the valve opens and closes more fully.
Bicuspid aortic valve repair may be an option to treat leaky valves, but it cannot be used to treat a stenotic or narrowed bicuspid aortic valve.
Bicuspid aortic valve repair can be performed with a minimally invasive “J” incision surgical technique.
Aortic valve surgery is technically difficult and must be performed by a surgeon experienced in aortic valve repair.
Repair of an enlarged aorta
Aortic valve disease is often associated with an enlargement (aneurysm) of the ascending aorta, the initial part of the aorta (the body’s main blood vessel that originates from the aortic valve).
If the aorta is very enlarged (usually more than 4.5 to 5 cm in diameter), this part of the aorta may need to be replaced.
The replacement is performed at the time of repair or replacement of the aortic valve.
In patients who have a defective aortic valve and an enlarged aorta, a special procedure (David procedure) may be done.
David’s procedure allows surgeons to repair the aortic valve and simultaneously replace the enlarged ascending aorta.
Repair of lacerations or valve holes
Also, if the valve leaflets have tears or holes, the surgeon can stitch them up with tissue patches.
Aortic valve replacement
If valve repair is not an option, the surgeon may replace the valve.
The native (original) valve is removed and a new valve is stitched to the annulus of the native valve.
The new valve can be mechanical or biological.
Biological valve replacement
Most aortic valves are replaced with a bioprosthesis.
Tissue valves (also called tissue or bioprosthetic valves) are made from tissue, but may also have artificial parts to provide additional support and allow the valve to be stitched in place.
About 80% of aortic valves are replaced with a bioprosthesis.
Tissue valves can be made from pork (swine) tissue, bovine (bovine) pericardial tissue, or pericardial tissue from other species.
These valves are safe to insert, last a long time (15 to 20 years), and allow patients to avoid the use of anticoagulants (blood thinning drugs) for life.
Replacement of the aortic valve with a human homograft (also called allograft)
A homograft is an aortic or pulmonary valve taken from a donated human heart, stored, treated with antibiotics, and frozen under sterile conditions.
Homografts are mostly used when the aortic root is destroyed by endocarditis (infection).
Replacement of mechanical valves
Mechanical valves are made entirely of mechanical parts, non-reactive and well tolerated by the body.
The bileaflet valve is the most commonly used.
It consists of two sheets of pyrolytic carbon (diamond-like quality) in a ring covered with a polyester fabric.
All patients with mechanical valve prosthetics should take the blood-thinning drug, warfarin (Coumadin), for the rest of their lives to reduce the risk of blood clotting and stroke.
This increases the risk of bleeding.
Ross procedure (also called switch procedure)
Ross’s operation is usually performed on patients under the age of 30 who wish to avoid lifelong use of blood thinners (blood thinning drugs) after surgery.
During this procedure, the patient’s normal pulmonary valve is removed and used to replace the diseased aortic valve.
The pulmonary valve is then replaced with a pulmonary homograft.
Ross’s surgery leaves two valves at potential risk of subsequent failure.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Aorta Surgery: What It Is, When It Is Essential
Abdominal Aortic Aneurysm: Symptoms, Evaluation And Treatment
Coronary Artery Bypass Surgery: What It Is And When To Use It
Do You Have To Face Surgery? Post-Surgery Complications
What Is Aortic Regurgitation? An Overview
Diseases Of The Valves Of The Heart: Aortic Stenosis
Interventricular Septal Defect: What It Is, Causes, Symptoms, Diagnosis, And Treatment
Heart Disease: The Atrial Septal Defect
Interventricular Defect: Classification, Symptoms, Diagnosis And Treatment
Arrhythmias: The Alterations Of The Heart
Identifying Tachycardias: What It Is, What It Causes And How To Intervene On A Tachycardia
Cardiac Rhythm Disturbance Emergencies: The Experience Of US Rescuers
Cardiomyopathies: Definition, Causes, Symptoms, Diagnosis And Treatment
How To Use An AED On A Child And An Infant: The Paediatric Defibrillator



