Autoimmune diseases: Myasthenia Gravis
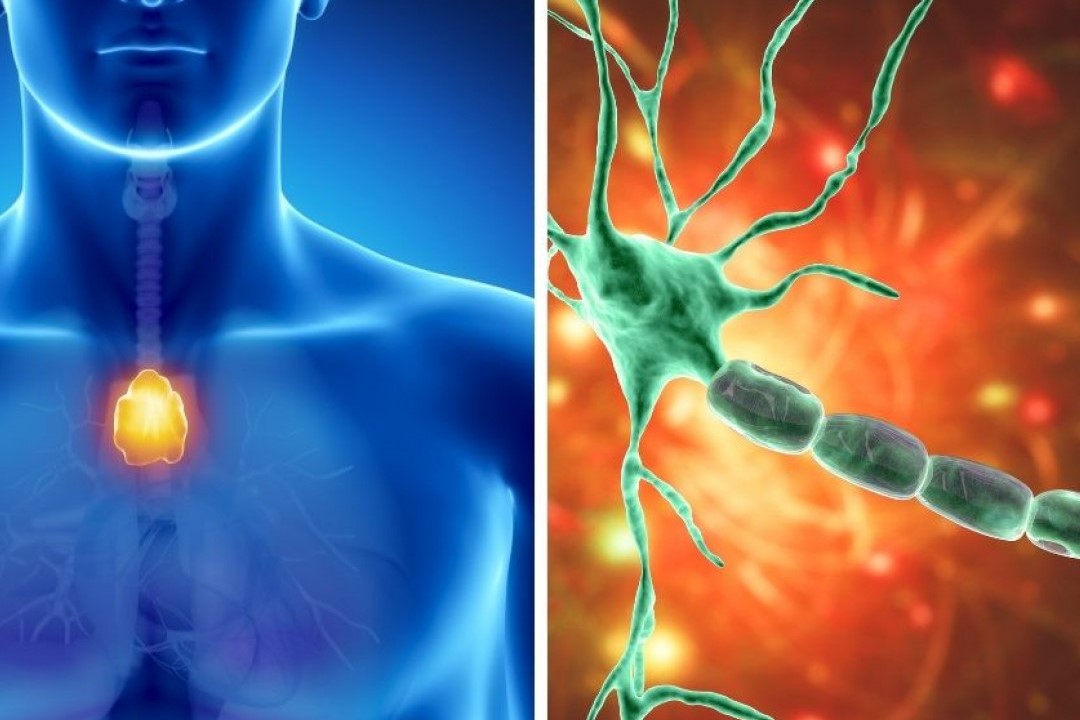
Myasthenia gravis is an autoimmune disease characterised by weakness and fatigue of the skeletal muscles, fatigue that decreases after a period of rest
It can present itself as a localised form in certain muscle groups or as a generalised form.
The incidence is 50-142 cases per million inhabitants.
MG is caused by a reduction in the number of postsynaptic acetylcholine receptors at the neuromuscular junction, such that they are insufficient to stimulate effective contraction of the muscle.
How does Myasthenia Grave manifest itself?
The characteristic feature of myasthenia is fatigue of the voluntary muscles.
It generally begins with fatigue of the extraocular muscles and the symptom of double vision (diplopia) or abnormal drooping of the upper eyelid (ptosis) (ocular myasthenia, 15% of cases).
In other cases, other muscles of the head are also involved, with difficulty articulating words, chewing or swallowing.
In most cases, these are generalised forms, which can also involve the breathing muscles and can worsen suddenly (myasthenic crisis) with the intake of certain drugs, during febrile states of a different cause or with anaesthesia.
85% of patients evolve towards a generalised form involving all skeletal muscles up to respiratory failure.
In 10-15% of patients, a benign tumour-like pathology of the thymus (thymoma) is present.
How is the diagnosis made?
The diagnosis of myasthenia can be confirmed by certain tests.
One of the main tests is the edrophonium test, the administration of which increases the concentration of acetylcholine at the level of the neuromuscular plate, thereby increasing muscle strength.
Electromyography is also used in the diagnosis of myasthenia gravis.
In addition, it is possible to test serum for anti-acetylcholine antibodies.
How is it treated?
The treatment of MG can be medical and/or surgical.
Medical treatment involves the administration of drugs (pyridostigmine) that inhibit acetylcholine degradation and thus improve neuromuscular transmission, and immunosuppressive therapy (cortisone, azathioprine, cyclosporine).
In generalised forms with respiratory paralysis, plasmapheresis or immunoglobulin treatment is useful in the acute phase.
In forms in which the presence of a thymoma is also associated, surgical removal of the thymus neoformation may be necessary.
Can a patient with myasthenia gravis undergo anaesthesia?
Certainly yes.
Anaesthesia treatment in a known myasthenic patient can be conducted with due consideration of a set of elements that must tend to avoid an aggravation of the disease or precipitate an acute myasthenic crisis.
First of all, a preoperative assessment of respiratory muscle function through respiratory function tests must be carried out, anxiolytic drugs and opioids (morphine and the like) must be avoided during preanaesthesia, and myasthenia therapy must be continued until the day of the surgical procedure.
Whenever possible, preference should be given to locoregional anaesthesia techniques while avoiding the use of certain types of local anaesthetics (esters).
The postoperative course requires close supervision in a dedicated area (intensive or sub-intensive care).
Numerous anaesthesiological techniques have been proposed in the treatment of myasthenic patients, but none has proved superior to the others.
Some prefer to avoid drugs that interfere at the neuromuscular junction (muscle relaxants) by resorting to powerful gaseous anaesthetics administered by inhalation.
Others use very small doses of non-prolonged-acting muscle relaxants.
Techniques that make use of drugs administered only intravenously have also been proposed, as potent substances with a very short duration of action are now available.
However, myasthenia gravis is a disease with many implications for proper anaesthetic conduct
The risk of impaired respiratory function in these patients requires the anaesthetist caring for them to be familiar with the problems of the disease, as well as all the pharmacological interactions that drugs, anaesthetic or otherwise, can have with myasthenia gravis.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Autoimmune Diseases: The Sand In The Eyes Of Sjögren’s Syndrome
Symptoms And Treatment For Hypothyroidism
Lymphangiomas And Lymphatic Malformations: What They Are, How To Treat Them
Lymphadenomegaly: What To Do In Case Of Enlarged Lymph Nodes
Retinal Thrombosis: Symptoms, Diagnosis And Treatment Of Retinal Vessel Occlusion
What Is Ocular Myasthenia Gravis And How Is It Treated?
Hashimoto’s Thyroiditis: What It Is And How To Treat It
What Is Macular Pucker And What Are The Symptoms



