Cervical dysplasia: what are the risk factors and how to treat it
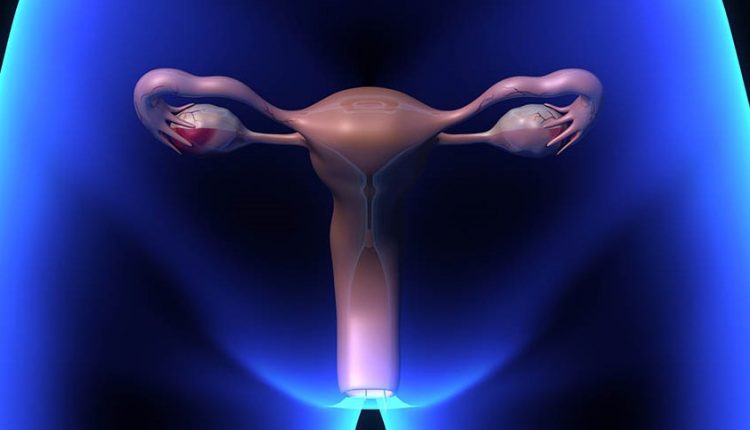
Cervical dysplasia is an abnormal and disordered growth of the superficial cells of the cervix. The term ‘plasia’ means growth
‘Dysplasia’ therefore means disordered cell growth
To better understand the meaning of this term, it is useful to first examine a normal cervix.
When one looks under the microscope at the superficial cell lining, i.e. the epithelium of a normal cervix, one sees layers of cells.
The normal distribution is such that the deepest layer consists of young, rounded cells that in their maturing process move towards the surface and assume a progressively flatter shape.
The surface is thus made up of flat cells.
In dysplasia, this organised growth process is missing
In mild dysplasia (CIN 1 – LSIL), the disorder only affects the cells of the deepest layer of the epithelium, which appear abnormal.
In moderate dysplasia (CIN 2 – HSIL), abnormal cells involve up to two-thirds of the lining of the cervical epithelium.
In severe dysplasia and/or carcinoma in situ (CIN 3 -HSIL), the entire thickness of the epithelium is disordered, but the abnormal cells have not yet spread below the ‘base’ of the epithelium.
Cervical dysplasia is also called a ‘precancerous lesion’ because it temporally precedes Uterine Neck Cancer
In invasive cancer, in fact, not only is the entire thickness of the epithelium disordered, but the abnormal cells have penetrated beyond the ‘basement’ of the epithelium, spreading into the underlying stromal tissue.
From this location, the abnormal cells can ‘metastasise’ i.e. migrate to other parts of the body, via the blood and/or lymphatic channels.
Invasive cancer is treated completely differently from dysplasia.
Why do I get cervical dysplasia?
There are a number of risk factors for cervical dysplasia.
They include sexual promiscuity, a history of genital infection with viruses such as Herpes and human papilloma virus (HPV), smoking, and the use of drugs that suppress the immune system (radiotherapy, cortisone).
Women who develop cervical dysplasia may also have only some or none of these risk factors.
Currently the most common risk factor for cervical dysplasia is genital infection with the human papilloma virus (HPV), which is usually (but not always) transmitted through sexual intercourse.
Some types of HPV can cause condylomata, i.e. small skin growths with a cauliflower-like appearance located on the skin of the vulva, the perianal area, the surface of the vagina, the cervix, or in the male partner.
Other HPV types, on the other hand, are capable of ‘transforming’ the cells of the cervix so as to facilitate the onset of dysplasia.
There is growing evidence that smoking is another important risk factor for cervical dysplasia
A woman who smokes, even occasionally, should stop smoking if she has cervical dysplasia.
Women with dysplasia who continue to smoke are not only more likely to develop recurrent cervical dysplasia despite adequate treatment, but also have an increased risk of developing dysplasia or cancer at other sites, including the vagina, vulva, lung, stomach, etc.
How is cervical dysplasia treated?
There are numerous treatment modalities for cervical dysplasia.
Factors influencing the choice of treatment include the extent and severity of the dysplasia, the woman’s age, her desire for future pregnancies, and the possible presence of other gynaecological problems.
The most common methods for treating cervical dysplasia are laser, LEEP, and surgical conization.
The aim of cervical dysplasia treatment, whether medical or surgical, is to remove the lesion and thus stop the cancer from developing.
Regardless of the treatment carried out, however, there is a possibility that the dysplasia may recur, i.e. that it may recur.
Usually, a recurrence is not a serious problem if it is discovered and treated early; however, it can develop into cancer, as can the primary lesion, if left untreated.
It is therefore essential to have regular check-ups (colposcopy) every 3 months during the first year after treatment, every 6 months the following year, and then once a year.
Treatment
Laser. The Carbonic Acid Laser uses a small infrared light beam to vaporise (destroy by turning into vapour) abnormal cells.
The laser beam is invisible to the human eye and is focused by the colposcope lens on a tiny dot (0.1-2 millimetres).
It is a very accurate technique as the area and depth of action of the laser beam can be controlled very precisely.
In fact, more than 90% of patients recover with a single treatment.
Numerous studies have shown that this method has no negative effect on fertility or pregnancy mechanisms.
It is a simple and painless method, which is performed under local anaesthesia.
Patients are usually given a painkiller in the 30 minutes preceding the treatment in order to inhibit any menstrual cramps following the treatment.
Bleeding, which is bothersome but rarely serious, may also appear occasionally.
LEEP (Loop Electrosurgical Excision Procedure).
LEEP means Loop Electrosurgical Excision Procedure.
A small, electrically charged loop is used to remove the dysplasia.
This technique is advantageous as it is performed quickly and provides a cone or cylinder sample that can later be analysed in the pathology laboratory.
It is also particularly useful for dysplasia extending to the endocervical canal.
It is performed under local anaesthesia.
Postoperative symptoms include menstrual-like cramps and generally contained bleeding.
Conisation (cone biopsy). Conisation is a surgical procedure by which a cone-shaped portion of the cervix is removed.
It is performed as an in-patient in a day-hospital setting and can be performed using a laser (laser coning), a scalpel (cold blade coning) or a macro-needle electrode and can be combined with a D&C (dilatation and curettage) to evaluate the higher cells in the uterus.
A coning may have diagnostic and/or therapeutic purposes: a cone performed for diagnostic purposes may, in some cases, simultaneously resolve the problem by completely removing the lesion that may be present on the biopsy tissue.
Conisation may sometimes be selected as the treatment of choice for dysplasia, especially if it significantly involves the cervical canal.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Colposcopy: How To Prepare, How It Is Performed, When It Is Important
How Does Cystitis Manifest Itself?
The Use Of Outpatient Hysteroscopy For Early Diagnosis
Accumulation Of Fluid In The Peritoneal Cavity: Possible Causes And Symptoms Of Ascites
What’s Causing Your Abdominal Pain And How To Treat It
Pelvic Varicocele: What It Is And How To Recognise The Symptoms
Can Endometriosis Cause Infertility?
Transvaginal Ultrasound: How It Works And Why It Is Important
Candida Albicans And Other Forms Of Vaginitis: Symptoms, Causes And Treatment
What Is Vulvovaginitis? Symptoms, Diagnosis And Treatment
Vaginal Infections: What Are The Symptoms?
Chlamydia: What Are The Symptoms And How To Treat It
Chlamydia, Symptoms And Prevention Of A Silent And Dangerous Infection
Drugs Used In Obstetric Emergencies To Modify Uterine Contractions
Total And Operative Hysterectomy: What They Are, What They Involve
Salpingitis: Causes And Complications Of This Fallopian Tube Inflammation
Hysterosalpingography: Preparation And Usefulness Of The Examination
Endometriosis: Symptoms, Diagnosis And Treatment
Pap Test, Or Pap Smear: What It Is And When To Do It
Gynaecological Cancers: What To Know To Prevent Them
Vulvodynia: What Are The Symptoms And How To Treat It
What Is Vulvodynia? Symptoms, Diagnosis And Treatment: Talk To The Expert



