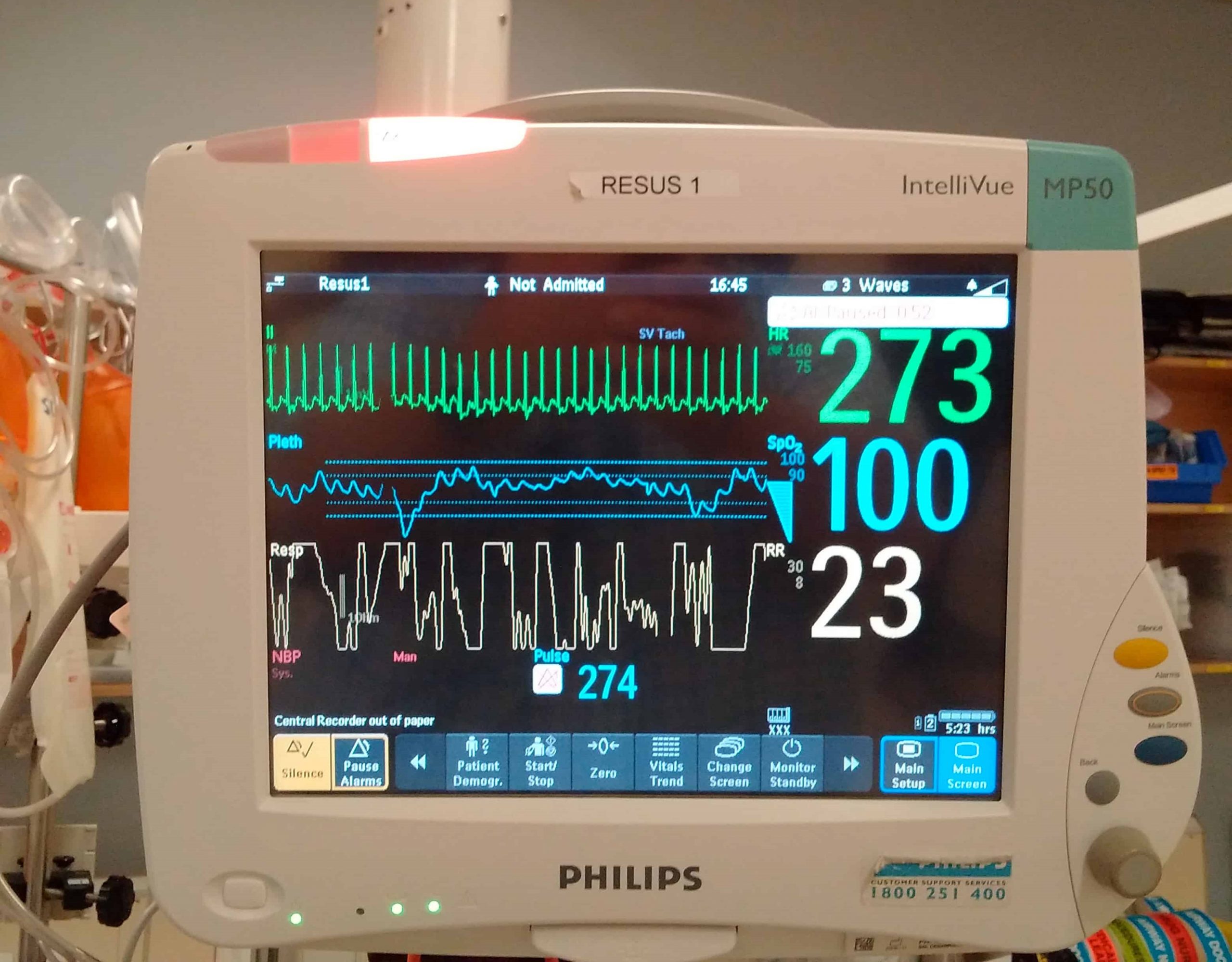
EMS: Pediatric SVT (Supraventricular tachycardia) vs Sinus Tachycardia
Supraventricular tachycardia (SVT) is a common non-arrest dysrhythmia seen in children, especially during infancy, and is the main cause of cardiac-related instability
Most infants with SVT will outgrow the syndrome without lasting effects. History of the complaint is the key to proper distinction between SVT and rapid sinus tachycardia.
CHILD HEALTH: LEARN MORE ABOUT MEDICHILD BY VISITING THE BOOTH AT EMERGENCY EXPO
The onset of SVT will usually show up in a normal child that is suddenly deteriorating with no history of a recent illness or injury. However, it must be carefully evaluated to ensure that proper treatment is implemented.
You do not want to cardiovert or administer adenosine to a child that is experiencing a fast sinus tachycardia and not SVT
Was the child sick? Think Sinus Tach! The best treatment modality will be aimed at discovering and correcting the underlying cause.
Don’t forget the H & T’s!
SVT v/s Sinus Tach in Pediatrics
- Patient History: The history of events leading up to calling for EMS assistance can offer valuable information in choosing the correct treatment modality for the child:
- Has the child been ill?
- Is he dehydrated?
- Is there bleeding that may be associated with shock?
- Does he have any known medical problems?
- Has this happened before and if so, what was done then to correct it?
- Does the child have any known drug allergies?
- Heart rate: Sustained heart rate during the event
- Infant: Sinus tachycardia is usually < 220 bpm; Supraventricular tachycardia is usually > 220 bpm
- Child: Sinus tachycardia is usually < 180 bpm; Supraventricular tachycardia is usually > 180 bpm
QUALITY AED? VISIT THE ZOLL BOOTH AT EMERGENCY EXPO
EKG Findings
Important EKG findings in pediatric sinus tachycardia:
- Heart rate will be < 220 bpm in an infant and < 180 bpm in children
- Variable R-R waves
- P waves present and upright in leads II, III, aVF
Sinus Tachycardia is normally secondary to:
- Dehydration
- Hypovolemia (most common)
- Fever
- Hypoxia
- Anemia
- Shocks
- Sinus Tach is not that uncommon in children but is normally caused by a contributing factor and not a true cardiac cause
Important EKG findings in pediatric supraventricular tachycardia:
- Heart rate will be > 220 bpm in infants and > 180 bpm in children
- Non-variable R-R waves
- The rhythm will be consistently regular (because associated AV block is extremely rare in infants/children)
- The P waves may be non-identifiable, especially when the ventricular rate is high
- If P waves are present, they will likely be inverted in leads II, III, and aVf
- QRS complex duration is 0.10 second in most cases
- SVT with QRS complex > 0.10 is extremely rare in infants and children
SVT seen in children may be of several types:
- Reentry with an accessory pathway (Wolf-Parkinson-White)
- Reentry without an accessory pathway
- Spontaneous depolarization of pacemaker sites
- Cardiac pathology (i.e: Ebstein’s anomaly)
- Pharmacological influences: (medications containing sympathomimetic amines, caffeine)
- Metabolic influences: (endocrine abnormalities, hyperthyroidism, etc.)
Symptoms/Management of Pediatric SVT
Signs and symptoms during supraventricular tachycardia are affected by the child’s age, duration of the SVT, prior ventricular function, and ventricular rate.
Infants with sustained episodes of SVT will present with:
- Tachypnea
- Loss of interest in feeding
- Irritability
- Progressing over 24-48 hours to lethargy
- Sternal and intercostal retractions
- Cardiovascular signs of a weak pulse, ashen color, etc.
If a child is hemodynamically stable and cooperative vagal maneuvers may be effective and are safest; such as:
- Ice water applied to the face
- Blowing through a straw
- Carotid sinus massage
An absolute contraindication to adenosine is sinus tachycardia (ST). Dehydrated patients, especially infants and young children with fever, failure to thrive, and/or an infection may appear to be in SVT, when in fact they’re barely compensated with a sinus tachycardia with a rate that may be greater than 180-200 bpm.
VISIT THE DMC DINAS MEDICAL CONSULTANTS BOOTH AT EMERGENCY EXPO
Patients that are experiencing rapid sinus tachycardia are at high risk for morbidity and mortality if adenosine is administered. Contact medical command early!
“Treat the patient and not the monitor”
- Emergency pharmacological therapy consists of Adenosine (0.1 mg/kg {max 1st dose 6 mg} by rapid bolus, may double 1st dose – 0.2 mg/kg {max 2nd dose 12 mg})
- Wolf-Parkinson-White (WPW) syndrome must be ruled out prior to treating as SVT
- Electrical emergency treatment includes Synchronized Cardioversion at 0.5 -1.0 joule/kg.
(Don’t forget to sedate prior to cardioversion when appropriate)
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Paediatric Toxicological Emergencies: Medical Intervention In Cases Of Paediatric Poisoning
Valvulopathies: Examining Heart Valve Problems
What Is The Difference Between Pacemaker And Subcutaneous Defibrillator?
Heart Disease: What Is Cardiomyopathy?
Inflammations Of The Heart: Myocarditis, Infective Endocarditis And Pericarditis
Heart Murmurs: What It Is And When To Be Concerned
Broken Heart Syndrome Is On The Rise: We Know Takotsubo Cardiomyopathy
Cardiomyopathies: What They Are And What Are The Treatments
Alcoholic And Arrhythmogenic Right Ventricular Cardiomyopathy
Difference Between Spontaneous, Electrical And Pharmacological Cardioversion
What Is Takotsubo Cardiomyopathy (Broken Heart Syndrome)?
Dilated Cardiomyopathy: What It Is, What Causes It And How It Is Treated
Heart Pacemaker: How Does It Work?
Basic Airway Assessment: An Overview
Assessment Of Abdominal Trauma: Inspection, Auscultation And Palpation Of The Patient
Pain Assessment: Which Parameters And Scales To Use When Rescuing And Treating A Patient
Airway Management After A Road Accident: An Overview
Tracheal Intubation: When, How And Why To Create An Artificial Airway For The Patient
What Is Traumatic Brain Injury (TBI)?
Acute Abdomen: Meaning, History, Diagnosis And Treatment
Poison Mushroom Poisoning: What To Do? How Does Poisoning Manifest Itself?
Chest Trauma: Clinical Aspects, Therapy, Airway And Ventilatory Assistance
The Quick And Dirty Guide To Pediatric Assessment


