Dilated cardiomyopathy: what it is, what causes it and how it is treated
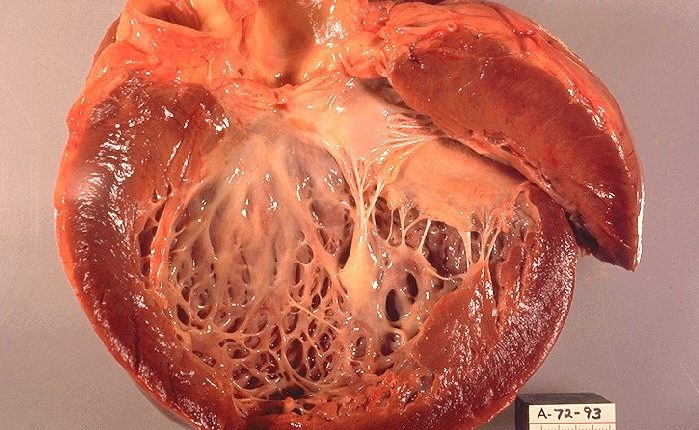
Dilated cardiomyopathy is a disease that affects the heart muscle and impairs the heart’s ability to efficiently pump blood to the rest of the body
What is dilated cardiomyopathy?
Dilated cardiomyopathy is a condition that mainly affects the left ventricle, the part of the heart that sends blood to the rest of the body via the aorta.
It is an enlargement of the ventricle, which is associated with a reduced ability to pump blood (‘systolic’ or ‘low ejection fraction’ heart failure).
Although it can be asymptomatic in some cases, dilated cardiomyopathy is a disease that, if left untreated, can over time lead to heart failure, a syndrome characterised by fluid accumulation in the lungs (pulmonary congestion), abdomen, legs and feet, mitral and/or tricuspid valve insufficiency (i.e. incontinence) secondary to ventricular dilation, embolisms, and arrhythmias that can also cause sudden death.
What are the causes of dilated cardiomyopathy?
In many cases it is not possible to trace the causes of the enlarged heart and dilated cardiomyopathy is therefore referred to as idiopathic.
There are several reasons why the heart can become enlarged: genetic mutations, congenital defects, infections, alcohol or drug abuse, certain chemotherapies, exposure to toxic substances such as lead, mercury and cobalt, and cardiovascular diseases such as ischaemic heart disease and high blood pressure.
What are the symptoms of dilated cardiomyopathy?
Generally, the symptoms of dilated cardiomyopathy are those of heart failure or are due to arrhythmias and may include skin paleness, weakness, easy fatigability, shortness of breath during even modest exertion or when lying down, a persistent dry cough (particularly when lying down), swelling of the abdomen, legs, feet and ankles, sudden weight gain caused by water retention, loss of appetite, palpitations, dizziness or fainting.
How to prevent dilated cardiomyopathy?
QUALITY AED? VISIT THE ZOLL BOOTH AT EMERGENCY EXPO
The risk of developing dilated cardiomyopathy can be reduced by avoiding smoking, consuming alcohol only in moderation, not using drugs, maintaining a healthy, balanced diet and regular exercise appropriate to one’s condition.
Diagnosis
In the presence of symptoms of a possible dilated cardiomyopathy, the doctor may prescribe the following tests:
- Blood tests: BNP (brain natriuretic peptide) can be measured, which is elevated in the presence of heart failure; alterations in liver and kidney function indices may be present, expressing the suffering of these organs due to heart failure; hyposodopaemia and anaemia are present in the most serious cases.
- Chest X-ray (chest X-ray): provides two important pieces of information: the first concerns the size of the heart and the second the presence and degree of pulmonary congestion.
- ECG: records the electrical activity of the heart. It can show multiple alterations, including signs of previous myocardial infarction or signs of overload (overwork fatigue) of the left ventricle or arrhythmias.
- Echocardiogram: This is an imaging test that visualises the structures of the heart and the functioning of its moving parts. The device sends a beam of ultrasound to the thorax, through a probe resting on its surface, and reprocesses the reflected ultrasounds which return to the same probe after interacting in different ways with the various components of the cardiac structure (myocardium, valves, cavities). It is the pivotal examination: it enables the size and thickness of the heart chamber walls, contractile function (measured by a parameter called ‘ejection fraction’) and valve function to be assessed, and pulmonary pressure to be estimated.
- Exercise test with oxygen consumption: the test consists of recording an electrocardiogram while the patient performs physical exercise, usually walking on a treadmill or pedalling on an exercise bike; a mouthpiece is also applied to measure exhaled gas. The test is conducted according to predefined protocols. It allows multiple pieces of information to be acquired, the most important of which are the subject’s resistance to exercise and the appearance of signs of ischaemia under stress.
- Coronarography: this is the examination that makes it possible to visualise the coronary arteries by injecting radiopaque contrast medium into them. The examination is performed in a special radiology room, in which all necessary sterility measures are observed. The injection of contrast into the coronary arteries involves the selective catheterisation of an artery and the advancement of a catheter to the origin of the explored vessels. It serves to exclude the presence of significant coronary artery disease.
- Cardiac catheterisation: invasive method based on the introduction of a small tube (catheter) into a blood vessel; the catheter is then pushed up to the heart and allows important information to be acquired on blood flow and oxygenation and pressure within the cardiac chambers and pulmonary arteries and veins. Performed infrequently; it documents increased ventricular filling pressures and, in more severe forms, reduced cardiac output (i.e. the amount of blood pumped by the heart) and pulmonary hypertension.
- Endomyocardial biopsy: this is performed during cardiac catheterisation using an instrument called a biotome. Biopsies are usually taken on the right side of the interventricular septum. It is indicated in patients with recent dilated cardiomyopathy and ‘fulminant’ heart failure to detect the presence of myocarditis and, if so, to identify the type of cells supporting the inflammatory process, as this has an important prognostic value.
- Cardiac magnetic resonance imaging (MRI) with contrast medium: produces detailed images of the structure of the heart and blood vessels by recording a signal emitted by cells subjected to an intense magnetic field. It provides the same information as the echocardiogram, but allows a better evaluation of the right ventricle, and, in addition, to assess the ‘structure’ of the myocardium, thus allowing the presence of inflammatory processes and areas of fibrosis (scarring) to be identified.
- CT heart scan with contrast medium: this is a diagnostic imaging examination that involves exposure to ionising radiation. It gives similar information to MRI. With current equipment, by administering contrast medium intravenously, it is then possible to reconstruct the coronary lumen and obtain information on any critical narrowing.
- Genetic investigations: these are carried out by analysing the DNA of white blood cells contained in a blood sample obtained from a normal venous sampling. In the case of familial dilated cardiomyopathies, it is possible to search for genetic mutations associated with the development of dilated cardiomyopathy; if a mutation associated with the development of dilated cardiomyopathy is identified, it will then be possible to study the ‘healthy’ relatives: those in whom the search for the mutation proves negative can be reassured that they will not develop the disease.
Treatments
When the cause of dilated cardiomyopathy is known, it should, if possible, be removed or corrected. Regardless of the cause, therapy for heart failure should be instituted to improve symptoms and increase survival.
Currently, therapy for heart failure includes:
- Medications: ACE-inhibitors/sartan, beta-blockers, anti-aldosteronics, diuretics, digoxin.
- Implantation of a biventricular pacemaker (PM) and/or an automatic defribrillator (ICD).
In more severe cases refractory to the above treatments: the implantation of left ventricular assist devices (LVAD) and/or heart transplantation.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Heart Disease: What Is Cardiomyopathy?
Inflammations Of The Heart: Myocarditis, Infective Endocarditis And Pericarditis
Heart Murmurs: What It Is And When To Be Concerned
Broken Heart Syndrome Is On The Rise: We Know Takotsubo Cardiomyopathy
Cardiomyopathies: What They Are And What Are The Treatments
Alcoholic And Arrhythmogenic Right Ventricular Cardiomyopathy
Difference Between Spontaneous, Electrical And Pharmacological Cardioversion
What Is Takotsubo Cardiomyopathy (Broken Heart Syndrome)?



