
Acute Appendicitis in Multisystem Inflammatory Syndrome in Children With COVID-19: case report from South Africa
Acute appendicitis, a case report from South Africa. The COVID-19 (PIMS-TS) related multisystemic inflammatory syndrome was perhaps the pediatric pathology linked to the coronavirus pandemic that has most questioned researchers around the world.
Initially confused with Kawasaki Syndrome, with which it shares an important part of the symptomatology, it is still the subject of studies today.
In an interesting publication on acute appendicitis in children in Australia with this syndrome appeared The Pediatric Infectious Disease Journal.
The case report “Acute Appendicitis in Multisystem Inflammatory Syndrome in Children With COVID-19” is signed by Lishman, Juanita FCPaed; Kohler, Charles MBChB, MRCS; de Vos, Corne FCPaedSurg; van der Zalm, Marieke M. PhD; Itana, Justina MBChB; Redfern, Andrew FCPaed; Smit, Liezl FCPaed; Rabie, Helena PhD
Case report from South Africa: Acute appendicitis in children with multisystem inflammatory syndrome by COVID-19
South Africa has the highest number of COVID-19 cases in Africa to date with Cape Town as the initial epicenter.
Up to 20 August 2020, 78 children with positive polymerase chain reaction (PCR) severe acute respiratory syndrome (SARS)-CoV-2 were admitted to Tygerberg Hospital in Cape Town.
We present 4 of these children, 5- to 12-years-old age (2 males) with appendicitis and confirmed SARS-CoV-2 on PCR of respiratory specimens (Table 1).
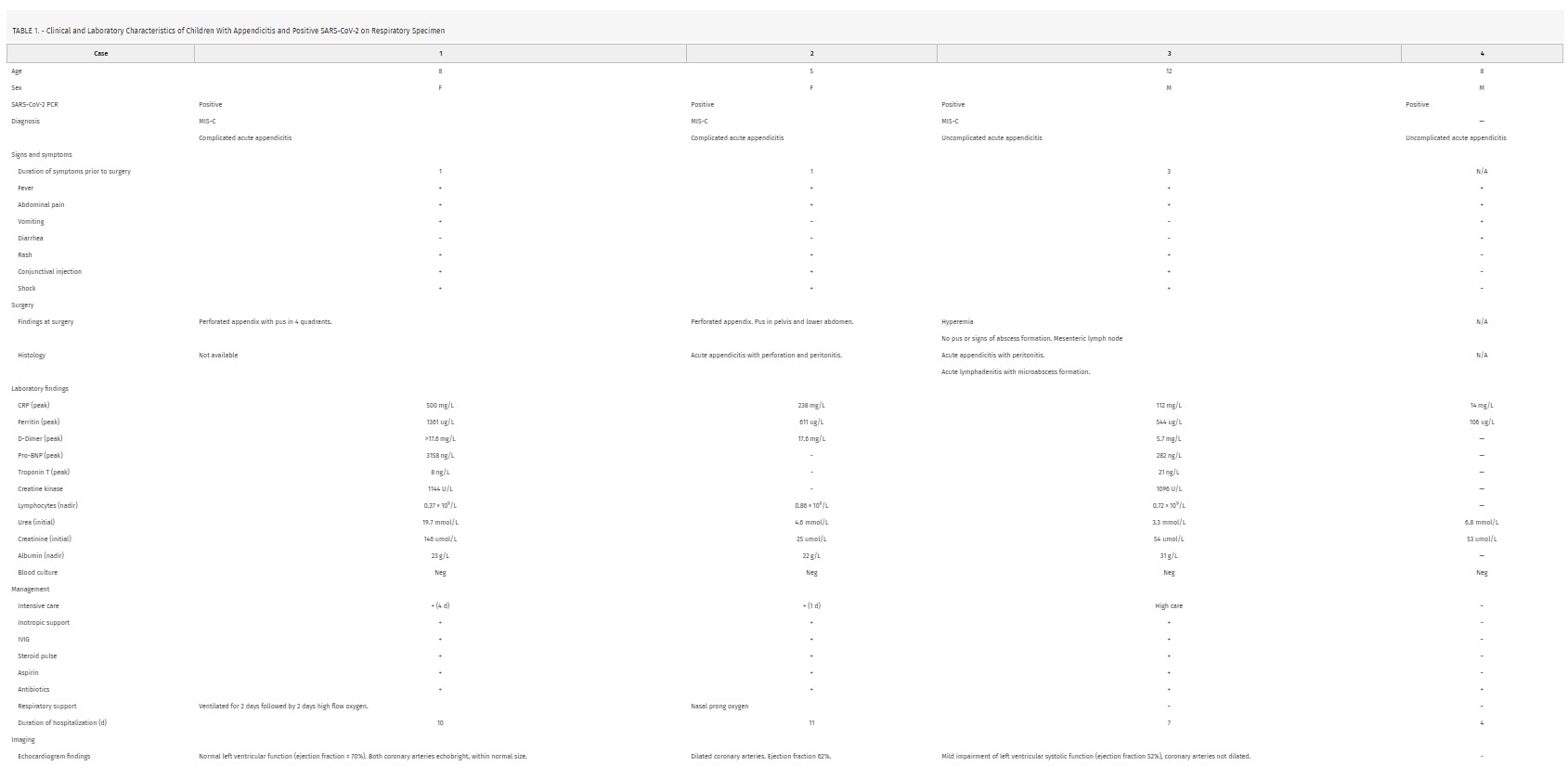 Three children were initially diagnosed with acute appendicitis and treated surgically and multisystem inflammatory syndrome in children (MIS-c) was diagnosed in all three after appendectomies.
Three children were initially diagnosed with acute appendicitis and treated surgically and multisystem inflammatory syndrome in children (MIS-c) was diagnosed in all three after appendectomies.
The fourth child was admitted with clinical appendicitis and tested for SARS-CoV-2 due to hospital policy but was managed non-surgically and did not have MIS-c.
Similar to a recent case series from London, we highlight that children with COVID-19 may present with clinical features suggestive of appendicitis or atypical appendicitis as part of MIS-c.
Cases 1 and 2 were included in a recent report on MIS-c in Cape Town, and all children were diagnosed with appendicitis during a time where an increase in these case was identified in our center.
However, unlike children from London, all children with MIS-c and appendicitis were PCR positive for SARS-CoV-2.
Moreover, children in the London series were diagnosed with terminal ileitis and none required surgery.
In our series of MIS-c, 3 of the children had surgically confirmed appendicitis (Table 1): 2 with complicated appendicitis with perforation and intra-abdominal pus and the third was confirmed histologically.
Acute appendicitis, a complication of COVID-19?
The possible relationship of viral entry through angiotensin-converting enzyme 2 receptors, abundantly present in the terminal ileum, and its relationship with terminal ileitis has been well documented.
What is not clear, is whether appendicitis may occur as a complication of SARS-CoV-2 through similar proposed mechanisms related to the inflammation associated with viral entry or reactive lymphoid hyperplasia causing luminal obstruction.
Acute appendicitis is known to be associated with Kawasaki disease, of which MIS-c shares many common clinical and pathologic features, possibly related to appendicular artery vasculitis.
In Kawasaki disease, abdominal features may represent more severe disease.5 No fecoliths were found in any of the children requiring appendectomy, possibly supporting inflammation or vasculitis as pathologic mechanism.
Where surgical emergencies are not managed in conjunction with pediatricians, surgeons should familiarize themselves with the features of MIS-c to facilitate early identification and referral of possible cases.
The importance includes the impact on diagnosis of appendicitis, postoperative recovery, and the management of multisystem involvement, which differentiates this entity from the regular course of isolated acute appendicitis.
Our experience suggests that, as with Kawasaki disease, pediatricians that diagnose MIS-c should be vigilant and continue to carefully evaluate children for surgical complications, including appendicitis and perforation, particularly if abdominal pain is part of the presenting complaint.
Access to sophisticated imaging to differentiating appendicitis from terminal ileitis may be limited in some settings, but if there is doubt the most sophisticated available imaging should be sought.
Our experience further highlights the suspected association between acute appendicitis, COVID-19, and MIS-c.
This should always be considered particularly in children with clinical appendicitis who are PCR positive for SARS-CoV-2 at the time of presentation.
“Acute Appendicitis in Multisystem Inflammatory Syndrome in Children With COVID-19″ on The Pediatric Infectious Disease Journal
Acute_Appendicitis_in_Multisystem_Inflammatory.40Read Also:
COVID-19, Discovered The Multisystem Inflammatory Syndrome Activation System



