Mitral regurgitation, discovering mitral insufficiency
Mitral regurgitation (or mitral insufficiency) is a heart disease that affects the mitral valve. This alteration implies that, during the ventricular contraction phase, the mitral valve, which should close hermetically to prevent blood from flowing back from the ventricle to the left atrium, remains partially open, allowing blood to flow back
A typical cause of mitral insufficiency is the alteration of some components of the valve itself such as lesions to the leaflets, the valve ring or the tendinous cords and the papillary muscles to which it is anchored.
It is easy to understand how a lesion of these structures leads to an imperfect closure of the valve orifice, with a reflux of blood during systole.
The problem induces a part of the blood, which would be destined for the spraying of the peripheral organs, to return towards the atrium, generating a condition of hypoperfusion which can result in organic decompensation.
What is the mitral valve used for?
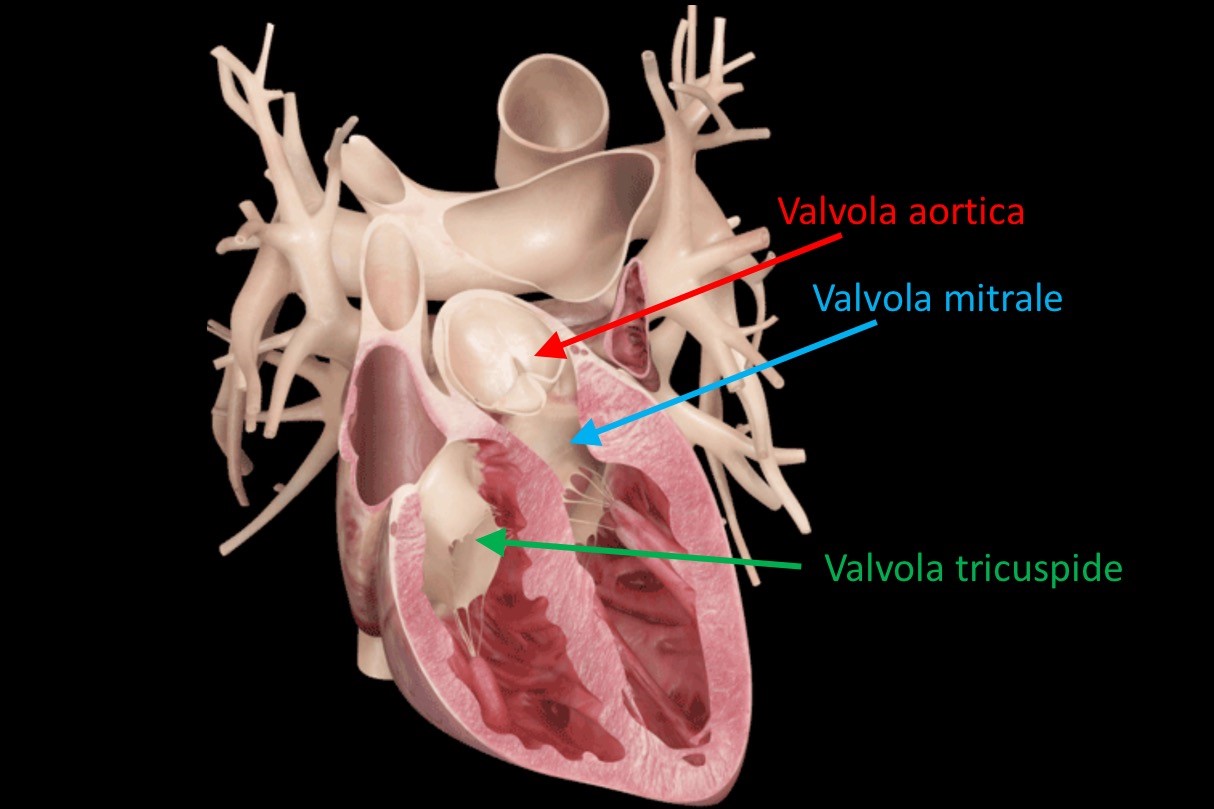
The mitral valve is a fibrous-based structure located between the left chambers of the heart (atrium and ventricle).
During ventricular systole, its job is to close hermetically to ensure that oxygenated blood flows unidirectionally from the ventricle to the aorta to be distributed throughout the body.
In a person with mitral regurgitation, this valve does not function properly and does not close completely, allowing some of the pumped blood to flow back from the ventricle to the atrium.
Mitral regurgitation is the typical effect of lesions to the different components of the mitral valve
The consequent reduction in cardiac output leads to a reduction in the inflow of oxygenated blood to peripheral organs with the possible development of heart failure.
Complications associated with mitral regurgitation include not only fatigue and general malaise, but also ventricular dilatation and hypertrophy, heart failure and abnormalities, arrhythmias such as atrial fibrillation, and diseases such as endocarditis.
Types of mitral regurgitation
Mitral valve dysfunction is classified according to its underlying cause and rate of onset.
Etiological classification
We speak of primary mitral regurgitation when the dysfunction is caused by alterations at the level of the mitral valve.
For example: lesion of the valve leaflets, lengthening or rupture of the tendon chordae and papillary muscles, calcification of the mitral annulus.
On the other hand, insufficiency is said to be secondary when the mitral valve itself is in good condition, but it is the left ventricle that shows structural alterations that lead to impaired valve closure.
This second type of mitral regurgitation usually appears following post-ischemic dilated heart disease.
Classification based on the speed of onset
Based on the speed with which the symptoms appear, mitral regurgitation can be acute – where the ventricle does not have time to adapt to the changes, because everything happens very quickly – or chronic, if the change is generated so slowly as to leave the heart time to adapt to the new hemodynamic condition.
Symptoms
The person affected by mitral insufficiency can present a set of symptoms, the onset of which can be sudden – if the dysfunction is acute – or gradual.
Dyspnea (difficulty breathing), especially with exertion, is the most common manifestation.
Cardiac output decreases and the organs no longer get the amount of blood necessary for their function.
In response, the body takes more breaths, causing a feeling of “shortness of breath”.
Another possible symptomatological manifestation is the alteration of the normal heartbeat, with palpitations and the onset of atrial fibrillation.
In addition to fatigue and general malaise, the subject may experience chest pain.
He may experience frequent fainting or develop symptoms which, at least initially, do not worry him or which he does not notice: cough, especially at night and in the supine position, swelling of the feet and ankles, weak and irregular pulse.
Mitral regurgitation can predispose to pulmonary edema, ischemia and infarction
Pulmonary edema is the direct consequence of the increase in blood pressure generated by mitral regurgitation.
If the problem sets in acutely, the left ventricle does not become hypertrophic as it does not have the time and therefore, to guarantee a sufficient range, it increases its operating pressures, also going to increase, by reflex, that of the pulmonary blood vessels.
Ischemias and infarctions are due to the inopportune triggering of the coagulation cascade.
Thrombi that form in conditions of turbulent flow and damage to the endothelial wall, disintegrate, releasing emboli that can obstruct blood flow in the vessels.
A typical sign of mitral regurgitation is the systolic murmur.
It is common for doctors to detect a heart murmur in these patients during the physical examination, which is heard as blood regurgitates from the left ventricle into the atrium.
Identifying the type of mitral regurgitation is crucial since acute regurgitation and chronic regurgitation require different treatment modalities.
The causes
Lesions that are created at the level of the mitral valve can have various causes.
Here are the most common:
- infective endocarditis;
- acute rheumatic endocarditis;
- coronary artery disease and vascular problems (typical is the slow calcification of blood vessels);
- malfunction of a previously implanted pacemaker, atrial defibrillator, or prosthetic valve;
- collagen diseases;
- cardiac ischemia;
- congenital pathologies;
- valve fissure and mitral valve prolapse;
- connect.
Diagnosis of mitral regurgitation
The diagnostic process to detect the presence of mitral regurgitation starts from the patient’s suspicion that he reports the presence of some symptoms.
These are usually not specific to the condition and it is therefore essential for the doctor to request a series of diagnostic tests aimed at evaluating the possible presence of the pathology.
Let’s see together which are the most used techniques:
Electrocardiogram (ECG)
The electrocardiogram detects the electrical activity of the heart, returning it in the form of a waveform.
In this way it is possible to identify the possible presence of alterations that may be related to mitral regurgitation.
Atrial dilatation can induce both the development of atrial fibrillation and mitral regurgitation
In the patient presenting this rhythm anomaly, it is advisable to carry out further investigations to obtain structural information.
At the request of the cardiologist, the ECG can also be performed under stress.
The electrical activity of the heart is measured while the patient exercises, usually through the use of a treadmill or stationary bike.
Echocardiography
Echocardiography is an investigation that allows you to evaluate the heart structure.
Taking advantage of ultrasound, it allows you to image the areas of the heart (atria, ventricles, valves) and allows you to check their state of health.
With this technique it is possible to evaluate the dimensions of the chambers, evaluate the cardiac dynamics and detect the possible presence of mitral regurgitation.
In this way it is also possible to estimate the degree of valve insufficiency, allowing patients to be classified according to the severity of their condition.
Echocardiography can be transesophageal, if the examination is performed through the introduction of a probe that reaches the esophagus, or transthoracic.
It is a more in-depth technique because it directly evaluates not only the valvular condition, but also the extent of the insufficiency, the structure of the atria and ventricles and their residual contraction capacity.
Chest x-ray
A chest x-ray can be useful to see if the insufficiency has caused lung problems, such as edema.
It is an exam that also shows the anatomical changes typical of mitral dysfunction: dilating left atrium, left ventricular hypertrophy and possible calcifications of the mitral valve.
Stethoscopy
Stethoscopy is the diagnostic technique that, during the physical examination, allows you to hear the mitral murmur which corresponds to the regurgitation that occurs when the blood flows back from the ventricle to the left atrium.
MRI of the heart with MDC
This technique, which uses magnetic fields, provides detailed images of the heart and blood vessels and is the gold standard for structural assessment of heart muscle.
It requires the administration of an intravenous contrast fluid which highlights the various structures being studied.
Coronary angiography and cardiac catheterization
Coronary angiography, performed with the cardiac catheterization technique, is a more invasive examination than the previous ones.
A small catheter is inserted into a peripheral artery and pushed up to the heart chambers.
Through the introduction of contrast medium, it will be possible to evaluate any alterations in blood flow both in the heart chambers and in the coronary arteries.
The technique, in addition to having a fundamental diagnostic importance, is also useful for therapeutic purposes.
The most effective treatments
The choice of the most suitable treatment differs from patient to patient, based on the severity of the symptoms, their state of health and the etiology of the mitral regurgitation.
Mild mitral insufficiency is generally asymptomatic and requires only a few small precautions to limit the risk of cardiovascular complications.
For this reason it is necessary to perform periodic cardiological checks.
On the contrary, to treat moderate mitral regurgitation, it will be necessary to set up a pharmacological therapy.
In general, the most commonly used drugs are antihypertensive drugs, aimed at reducing blood pressure.
For this purpose, the doctor prescribes ACE inhibitors and/or diuretics.
All vasodilators, acting on the reduction of ventricular pressure, indirectly control the extent of regurgitation.
Finally, if the mitral dysfunction is severe and frankly symptomatic, surgical treatment will be mandatory.
The most used and effective techniques involve the replacement of the mitral valve with a mechanical or biological prosthesis or the direct repair of the valve itself.
Prognosis and complications related to mitral regurgitation
Mitral regurgitation has a variable prognosis based on the stage at which it is diagnosed.
When it is mild, and treated early, it is possible to control the condition and reduce the incidence of long-term complications.
On the contrary, in the more advanced stages or if the pathology is underestimated, serious complications may occur such as:
- Heart failure. The heart does not pump enough blood and lacks the adequate amount of oxygen and nutrients required by the organs.
- Pulmonary edema and pulmonary hypertension. Generally, when the pulmonary pressure becomes very high, it is not uncommon to have an accumulation of fluid in the alveolar level and to experience difficulty breathing.
- Mitral regurgitation can lead to the development of arrhythmias, in particular atrial fibrillation. The atria contract too quickly and irregularly. The blood does not flow correctly and the formation of thrombi is favored which can embolise, hindering the passage of blood into the vessels.
- Endocarditis. Individuals with mitral regurgitation are predisposed to the development of inflammatory diseases of the inner wall of the heart.
These are serious complications that must be treated promptly, as they can lead the subject to cardiac arrest.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Ventricular Fibrillation Is One Of The Most Serious Cardiac Arrhythmias: Let’s Find Out About It
Atrial Flutter: Definition, Causes, Symptoms, Diagnosis And Treatment
Know The Symptoms Of Heart Attack And 5 Ways To Prevent It
Patent Foramen Ovale: Definition, Symptoms, Diagnosis And Consequences
Sinus Tachycardia: What It Is And How To Treat It
Inflammations Of The Heart: Myocarditis, Infective Endocarditis And Pericarditis
Aorta Surgery: What It Is, When It Is Essential
Abdominal Aortic Aneurysm: Symptoms, Evaluation And Treatment
Spontaneous Coronary Artery Dissection, Which Heart Disease Is Associated With
Coronary Artery Bypass Surgery: What It Is And When To Use It
Do You Have To Face Surgery? Post-Surgery Complications
What Is Aortic Regurgitation? An Overview
Diseases Of The Valves Of The Heart: Aortic Stenosis
Interventricular Septal Defect: What It Is, Causes, Symptoms, Diagnosis, And Treatment
Heart Disease: The Atrial Septal Defect
Interventricular Defect: Classification, Symptoms, Diagnosis And Treatment
Arrhythmias: The Alterations Of The Heart
Identifying Tachycardias: What It Is, What It Causes And How To Intervene On A Tachycardia
Cardiac Rhythm Disturbance Emergencies: The Experience Of US Rescuers
Cardiomyopathies: Definition, Causes, Symptoms, Diagnosis And Treatment
How To Use An AED On A Child And An Infant: The Paediatric Defibrillator
Aortic Valve Surgery: An Overview
Cutaneous Manifestations Of Bacterial Endocarditis: Osler Nodes And Janeway’s Lesions
Bacterial Endocarditis: Prophylaxis In Children And Adults
Infective Endocarditis: Definition, Symptoms, Diagnosis And Treatment



