Pulmonary embolism: symptoms and treatment
Pulmonary embolism is in most cases the complication of a deep vein thrombosis of the lower limbs; it occurs when more or less large fragments detach from a thrombus formed in a deep vein
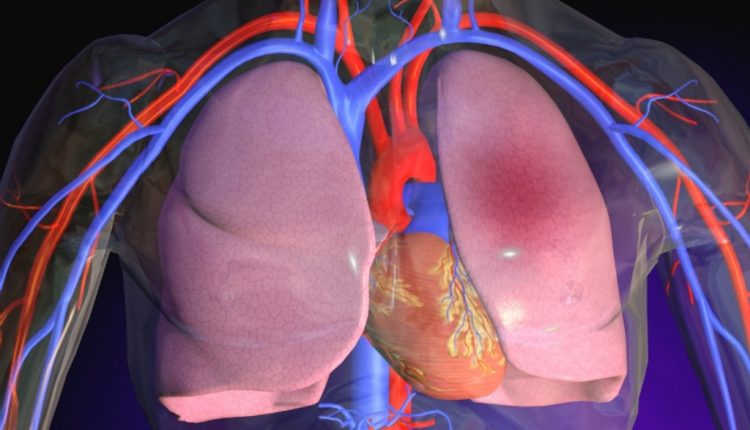
These clot fragments (emboli) are carried by the bloodstream in increasingly larger vessels to the heart, which in turn pushes them into the arteries of the lung.
Here, the blood vessels narrow again and the clots stop, causing an obstruction.
Sometimes pulmonary embolism is a consequence of deep vein thrombosis of the upper limb (rare) or of other districts (e.g. the pelvis)
The risk of pulmonary embolism is much higher if the thrombosis is not promptly diagnosed and not adequately treated: it is estimated that in the absence of proper anticoagulant therapy, more than 40% of deep vein thromboses result in pulmonary embolism.
Pulmonary embolism is the third leading cause of acute cardiovascular disease and affects one in a hundred thousand people in Italy.
Mortality within thirty days of diagnosis is over 10%.
It should be pointed out that pulmonary embolism due to thrombosis has nothing to do with embolism affecting divers, which is caused by the formation of gas bubbles in the blood.
Pulmonary embolism, what damage does it cause?
The severity of pulmonary embolism depends on both the extent and the district affected, as well as the patient’s ‘basic’ cardiovascular condition.
It can affect the pulmonary microcirculation (microembolism), but also the large vessels (massive embolism).
A massive pulmonary embolism involves the obstruction of several vessels of the pulmonary arterial tree, but also that of a single large-calibre vessel and can lead to severe respiratory and cardiac failure.
If, on the other hand, the embolus or emboli are small, such that they only reach the peripheral vessels, only the pulmonary segment supplied by these vessels may be partially compromised and the patient may even remain asymptomatic.
In some cases, the embolism complicates with pulmonary infarction and superimposed bronchopneumonia: it is manifested by sputum of blood-streaked phlegm.
Since pulmonary embolism is a complication of deep vein thrombosis, the risk factors are the same as those indicated for deep vein thrombosis: age, family history, diabetes, taking the contraceptive pill, pregnancy and puerperium, trauma (especially lower limb fractures), myocardial infarction and heart failure, previous thromboembolic episodes, and malignant neoplasms.
It should also be remembered that surgery and long periods of immobilisation can cause deep vein thrombosis.
Since pulmonary embolism originates from deep vein thrombosis, even asymptomatic, its frequency is remarkably high in patients hospitalised for any reason and it has been found to be the leading cause of death in patients who have undergone surgery.
Or it can affect those who travel by plane for a long time and are forced to keep their lower limbs immobile.
For this reason, it is very important to move and exercise the legs.
Symptomatology of pulmonary embolism
Symptoms can vary greatly: in microembolism, the patient may experience almost no discomfort; massive embolism, on the other hand, presents dramatically, with shortness of breath, coughing, chest pain.
Sometimes the onset of symptoms is very violent, sometimes resulting in death.
Pulmonary embolism can also have an asymptomatic course.
When present, the symptomatology is non-specific and is similar to that of many other cardio-respiratory diseases.
The most common typical signs are tachypnoea and tachycardia, followed by chest pain, which may be of varying degrees, localised or diffuse.
The patient often complains of anxiety, dyspnoea (feeling of breathlessness), chest pain, cardiovascular collapse (if there is a reduction in blood flow and consequent hypotension), transient drops in blood flow to the brain (cerebral hypoafflux).
The patient may appear cyanotic or present in a febrile state
Right ventricular insufficiency may occur in the heart, resulting in an increased heart rate (galloping rhythm).
Increased jugular venous pressure causes swelling and reddening of the vessels in the neck.
The diagnosis of pulmonary embolism is never simple: the examinations that are most reliable are AngioTAC (which alone can resolve most diagnostic doubts even in the case of minimal embolisms), pulmonary scintigraphy (a special substance is injected into a vein that diffuses into the lungs and is detected by special equipment) or angiography (a ‘contrast medium’ is injected into the pulmonary artery, the movements of which can be detected by a series of X-rays).
These are not simple investigations that can be performed anywhere.
The other investigations, such as the electrocardiogram and laboratory tests, can be helpful in clarifying certain ideas, but are rarely conclusive.
Therefore, it is only the doctor who, by carefully assessing the patient’s symptoms, can request the most appropriate examination.
Possible remedies against pulmonary embolism
Remedies against pulmonary embolism can be very effective: anticoagulant drugs and thrombolytics (those that dissolve thrombi), if used correctly and, above all, promptly, lead to excellent results; in particular situations, even surgery to remove the embolus may prove necessary.
One can therefore recover very well from pulmonary embolism, often without unpleasant ‘after-effects’ in the years to follow, but, as mentioned, one can also die of thrombosis.
Since diagnosis is not easy and one does not always have time to intervene, the most effective policy is to prevent.
Special attention deserves those people who have a tendency to thrombosis due to increased blood coagulability.
Specialised centres are able in many cases to identify even among apparently healthy people, who have close relatives with repeated thrombosis episodes, those most prone to deep vein thrombosis or pulmonary embolism.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Pulmonary Emphysema: Symptoms, Diagnosis And Treatment
Airway Management After A Road Accident: An Overview
Tracheal Intubation: When, How And Why To Create An Artificial Airway For The Patient
What Is Transient Tachypnoea Of The Newborn, Or Neonatal Wet Lung Syndrome?
Traumatic Pneumothorax: Symptoms, Diagnosis And Treatment
Diagnosis Of Tension Pneumothorax In The Field: Suction Or Blowing?
Pneumothorax And Pneumomediastinum: Rescuing The Patient With Pulmonary Barotrauma
Cervical Collar In Trauma Patients In Emergency Medicine: When To Use It, Why It Is Important
KED Extrication Device For Trauma Extraction: What It Is And How To Use It
ABC, ABCD And ABCDE Rule In Emergency Medicine: What The Rescuer Must Do
Multiple Rib Fracture, Flail Chest (Rib Volet) And Pneumothorax: An Overview
Primary, Secondary And Hypertensive Spontaneous Pneumothorax: Causes, Symptoms, Treatment
Pneumothorax And Haemothorax: Trauma To The Thoracic Cavity And Its Consequences
Spontaneous Pneumothorax: Discussing The Collapse Of The Lungs



