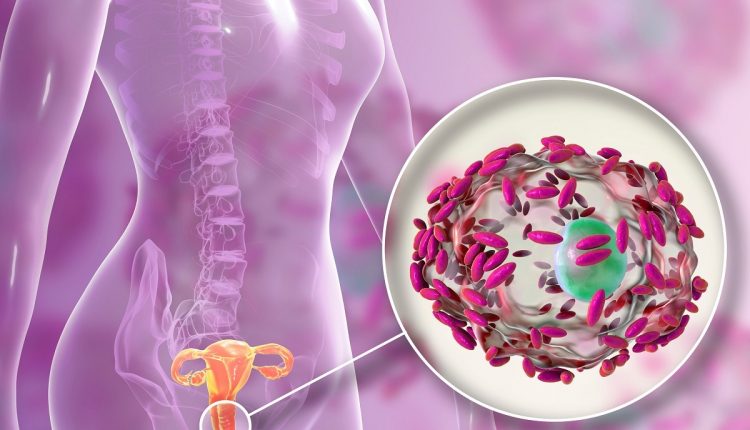
Bacterial vaginosis, how to defend yourself?
Bacterial vaginosis is part of vaginitis, i.e. infections affecting the female reproductive organ, and is characterized by an alteration of the normal vaginal pH
As with other parts of the body, the female genitals are physiologically rich in bacterial microorganisms which, if present in normal quantities, are benign and do not damage the normal ecosystem.
When the physiological vaginal bacterial flora (saprophytic flora in medical jargon) undergoes imbalances, secondary to internal or external ones that we will analyze, a real infection can arise.
Lactobacilli, benign bacteria that protect the vaginal mucosa, decrease and the white blood cells of the immune system come into play, because the whole environment is no longer protected, as there is generally a proliferation of harmful anaerobic bacteria.
An important index of good intimate health is represented by the pH
The vaginal environment is by nature moist and acidic, with pH values that remain between 3.8 and 4.5.
Acidity is essential, as it protects the vagina and counteracts humidity, which would favor the growth of pathogens.
Vaginitis is mostly common among sexually active women of childbearing age and, among these, bacterial vaginosis is the most frequent to contract.
It is important to treat it as soon as the symptoms are suspected because, if not treated in time, it can become complicated with much more serious gynecological problems.
Symptoms of bacterial vaginosis
Even if, in most cases, the infection initially presents itself as totally asymptomatic, here is a list of the main signs that can act as an alarm bell.
Intimate itching and burning. Patients with bacterial vaginosis almost always complain of an annoying intimate itching, which can also become burning, especially during urination phases.
Erythema and edema. The vaginal area may be red and swollen.
Since the intimate area is already heavily stressed due to the inflammatory state, it is easy to have difficulty or feel pain during sexual intercourse.
Increased vaginal discharge. It is the real typical symptom of bacterial vaginosis. These are also abundant losses, with a dirty white color, liquid or slightly sticky, but which have in common a bad smell reminiscent of fish.
Causes and risk factors of bacterial vaginosis
Bacterial vaginosis, as well as other infections affecting the same anatomical area, is still being studied by the medical community.
At the moment, the main bacteria that have been recognized as being able to stagnate between the vaginal walls by altering their pH are: Gardnerella vaginalis, Mycoplasma hominis, Mobiluncu spp. and Prevotella ssp.
To date it is not possible to draw up a list of unique and defined causes that lead to the development of the disease, but it is possible to identify a combination of factors that determine an increase in the proliferation of pathogens, with a consequent loss of the balance of the vaginal microbiome.
Assuming that every woman, at every stage of her intimate life, can suffer from bacterial vaginosis, here is a list of the main risk factors that predispose to a more probable onset of the disease.
Having unprotected sex. Vaginosis is more common in sexually active women. This is because sperm, coming into contact with the vagina, alters its normal pH. The intimate environment must prepare itself as more suitable to host sperm and a possible fertilized egg, so its acidity changes. A change in pH can lead, as we know, to abnormal bacteriological proliferation.
Likewise, casual relationships and relationships with a large number of partners increase the risk of vaginosis.
The use of mechanical intrauterine contraceptives can increase the risk of contracting vaginosis. The introduction of a foreign body into the vagina can in fact alter its normal ecosystem.
Some antibiotic therapies can modify the entire bacterial flora of the body, including the vaginal one, making it weaker in the face of the action of pathogens.
An excessive intimate hygiene rich in vaginal douching, often made with soaps that are too aggressive or with an incorrect pH, can paradoxically favor bacterial proliferation. For the same reasons, the use of particularly aggressive intimate deodorants is not recommended.
A possible cause of alteration of the intimate pH, and consequently of bacterial vaginosis, can be the use of detergents and softeners that are too aggressive for washing underwear; it is also not recommended to constantly wear too tight and synthetic underwear.
Stress and anxiety can affect the imbalances of the entire bacterial flora, including the vaginal one.
Finally, the vaginal pH can be modified by physiological changes that the body undergoes during the different stages of life, as occurs for example in the case of the menstrual cycle or pregnancy. During pregnancy, a vitamin D deficiency affects the normal functioning of the immune system. Deficient immune defenses can help the proliferation of bacteria of all kinds, even vaginal ones. If this deficiency is highlighted with blood tests, it will be the doctor’s job to suggest the right therapies for adequate reintegration.
The diagnosis of bacterial vaginosis generally occurs following a specialist gynecological evaluation
During the visit, the doctor will collect all the necessary information through the anamnesis, thus deepening the patient’s clinical history, questioning her about any present and past symptoms and trying to identify the presence of at least 3 out of 4 of the required diagnostic requirements and which we will deepen at brief (vaginal discharge, pH test, smell test, clue cells).
We can speak of bacterial vaginosis when, during direct observation of the genital organ, more or less abundant vaginal discharge emerges, dirty white, fluid or sticky.
The examination must also correspond to a vaginal pH greater than 4.5, a symptom of an ongoing infection.
The additional step of the physical examination includes taking a sample of these discharges to study them, observe their consistency and the responsible bacteria.
The collected substances, placed in contact with an alkaline substance such as potassium hydroxide, should release the typical smell of vaginosis (smell test).
The microscope study also allows you to see if there are clue cells or trace cells (i.e. if the normal vaginal cells are covered by bacteria), in addition to the white blood cells intervened to heal the infection.
Generally, bacterial vaginosis is a pathology that heals completely after appropriate therapy and without leading to complications or outcomes.
However, it must be kept in mind that, for a period, the vaginal flora is weakened and the probability of contracting sexually transmitted diseases rises.
Rarely, however, untreated or unresolved bacterial vaginosis can, over time, develop into pelvic inflammatory disease. have ectopic pregnancies and, in severe cases, infertility.
Similarly, vaginosis during pregnancy must be identified and treated immediately, since one of the main consequences is the risk of premature birth or miscarriage.
In fact, the infection could extend to the amniotic membrane, causing a risk of premature rupture.
Bacterial vaginosis, the most effective treatments
The task of prescribing the best treatment for bacterial vaginosis lies with the gynecologist, after careful observation of the symptoms and general state of health of the patient.
At the moment, the most used treatments are antibiotic drugs, prescribed with the aim of restoring the correct bacterial flora.
The most frequently used antibiotics exploit the properties of active ingredients such as metronidazole, clindamycin and secnidazole, which are introduced orally or applied to the vaginal walls using a topical method (creams, ointments, lotions).
In general, oral administration is the most prescribed, while topical application is reserved for pregnant women.
Those who opt for a treatment based on clindamycin are reminded that this substance has corrosive effects on the latex, therefore it is not suitable for practicing sexual intercourse with the use of a condom and vaginal diaphragm.
The choice of different contraceptive methods or an alternative therapeutic strategy is therefore recommended.
To make the intervention completely effective, it is recommended to combine the treatment with the intake of active ingredients that stimulate the production of lactobacilli, the so-called good bacteria that restore the balance of the vaginal flora orally or topically.
How to prevent it?
Preventing bacterial vaginosis 100% is not possible, but there are a number of best practices that help strengthen the immune system and limit the proliferation of harmful anaerobic bacteria.
Adopting a healthy lifestyle, based on a correct diet, is essential.
To be effective, the diet should be rich and varied. It is generally recommended to follow the Mediterranean diet.
Yes to fiber, fruit and vegetables.
The diet against bacterial vaginosis must then be attentive to the reintegration of probiotics for the restoration of the bacterial flora and the increase of lactobacilli.
For this reason, among the foods not to be missed on your tables, there are also yogurt and dairy products, lean meats, fish, olives and extra virgin olive oil for the dressing.
Avoid simple sugars contained in sweets and sugary drinks, alcohol, cheeses, foods rich in saturated fats and fried foods.
It is recommended, during the treatment phase, to avoid sexual intercourse to limit the possibility of contagion or infection.
It is also essential to maintain adequate care of intimate hygiene, without however undergoing too frequent vaginal washing and douching and with too aggressive and perfumed intimate detergents.
When choosing, it is always good to check that the pH is correct.
After each washing or water sport, make sure you dry completely and properly, following the line from vulva to anus and not vice versa, as the anal region is rich in faecal bacteria harmful to vaginal health.
Wear synthetic undergarments as little as possible, prefer cotton ones that are not too tight.
Change briefs, pantyliners and sanitary pads often, to limit the stagnation of bacteria and vaginal secretions.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
What Is Cervicalgia? The Importance Of Correct Posture At Work Or While Sleeping
Cervicalgia: Why Do We Have Neck Pain?
Cervical Stenosis: Definition, Causes, Symptoms, Diagnosis And Treatment
Cervical Stenosis: Symptoms, Causes, Diagnosis And Treatment
Cervical Collar In Trauma Patients In Emergency Medicine: When To Use It, Why It Is Important
Headaches And Dizziness: It Could Be Vestibular Migraine
Migraine And Tension-Type Headache: How To Distinguish Between Them?
First Aid: Distinguishing The Causes Of Dizziness, Knowing The Associated Pathologies
Paroxysmal Positional Vertigo (BPPV), What Is It?
Cervical Dizziness: How To Calm It Down With 7 Exercises
Back Pain: Is It Really A Medical Emergency?
Posture, The Mistakes That Lead To Cervicalgia And Other Spinal Pains
Lumbago: What It Is And How To Treat It
Lumbar Puncture: What Is A LP?
General Or Local A.? Discover The Different Types
Intubation Under A.: How Does It Work?
How Does Loco-Regional Anaesthesia Work?
Are Anaesthesiologists Fundamental For Air Ambulance Medicine?
Epidural For Pain Relief After Surgery
Lumbar Puncture: What Is A Spinal Tap?
Lumbar Puncture (Spinal Tap): What It Consists Of, What It Is Used For
What Is Lumbar Stenosis And How To Treat It
Lumbar Spinal Stenosis: Definition, Causes, Symptoms, Diagnosis And Treatment
Urethral Stenosis: Definition, Causes, Symptoms, Diagnosis And Treatment