Deep vein thrombosis: what it is, causes, treatment and patient management
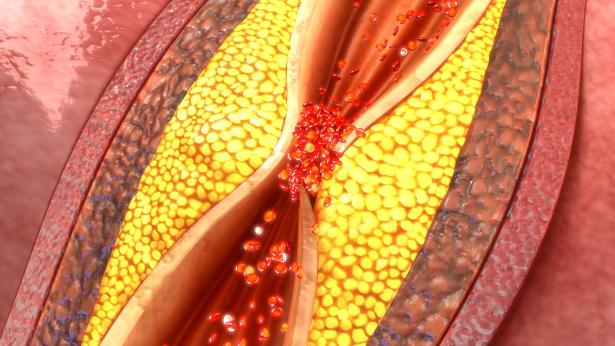
Deep vein thrombosis occurs when a blood clot (thrombus) forms in one or more of the deep veins in the body, usually in the legs
What is Deep Vein Thrombosis?
Deep vein thrombosis is a part of a condition called venous thromboembolism.
Deep vein thrombosis occurs when a blood clot (thrombus) forms in one or more of the deep veins in the body, usually in the legs.
Deep vein thrombosis can cause leg pain or swelling, but may occur without any symptoms.
Deep vein thrombosis is a serious condition because blood clots in the veins can break loose, travel through the bloodstream, and obstruct the lungs, blocking blood flow.
Although the exact cause of deep vein thrombosis remains unclear, there are mechanisms believed to play a significant role in its development
- Reduced blood flow. Venous stasis occurs when blood flow is reduced, when veins are dilated, and when skeletal muscle contraction is reduced.
- Damage. Damage to the intimal lining of blood vessels creates a site for clot formation.
- Phlebitis. Formation of a thrombus frequently accompanies phlebitis, which is an inflammation of the vein walls.
- Platelet aggregates. Venous thrombi are aggregates of platelets attached to the vein wall that have a tail-like appendage containing fibrin, white blood cells, and many red blood cells.
- Tail. The “tail” can grow or can propagate in the direction of the blood flow as successive layers of the thrombus form.
- Fragmentation. Fragmentation of the thrombus can occur spontaneously as it dissolves naturally, or it can occur with an elevated venous pressure.
- Recanalization. After an acute episode of DVT, recanalization or reestablishment of the lumen of the vessel typically occurs.
The incidences of deep vein thrombosis that occurs together with pulmonary embolism are:
The incidence of DVT is 10% to 20% in general medical patients, 20% to 50% in patients who have had stroke, and up to 80% in critically ill patients.
It is estimated that as many as 30% of patients hospitalized with DVT develop long-term post-thrombotic complications.
The exact cause of deep vein thrombosis remains unknown, but there are factors that may aggravate it further
- Direct trauma. Direct trauma to the vessels, as with fracture or dislocation, diseases of the veins, and chemical irritation of the veins from IV medications and solutions, can damage the veins.
- Blood coagulability. Increased blood coagulability occurs most commonly in patients for whom anticoagulant medications have been abruptly withdrawn.
- Oral contraceptives. Oral contraceptives use also lead to hypercoagulability.
- Pregnancy. Normal pregnancy is accompanied by an increase in clotting factors that may not return to baseline until longer than 8 weeks postpartum, increasing the risk of thrombosis.
- Repetitive motions. Repetitive motions may cause irritation to the vessel wall, causing inflammation and subsequent thrombosis.
A major problem associated with recognizing DVT is that the signs and symptoms are nonspecific
- Edema. With obstruction of the deep veins comes edema and swelling of the extremity because the outflow of venous blood is inhibited
- Phlegmasia cerulea dolens. Also called massive iliofemoral venous thrombosis, the entire extremity becomes massively swollen, tense, painful , and cool to the touch.
- Tenderness. Tenderness, which usually occurs later, is produced by inflammation of the vein wall and can be detected by gently palpating the affected extremity.
- Pulmonary embolus. In some cases, signs and symptoms of a pulmonary embolus are the first indication of DVT.
Deep vein thrombosis can be prevented, especially if patients who are considered high risk are identified and preventive measures are instituted without delay
- Graduated compression stockings. Compression stockings prevent dislodgement of the thrombus.
- Pneumatic compression device. Intermittent pneumatic compression devices increase blood velocity beyond that produced by the stockings.
- Leg exercises. Encourage early mobilization and leg exercises to keep the blood circulating adequately.
The following complications should be monitored and managed:
- Bleeding. The principal complication of anticoagulant therapy is spontaneous bleeding, and it can be detected by microscopic examination of urine.
- Thrombocytopenia. A complication of heparin therapy may be heparin-induced thrombocytopenia, which is defined as a sudden decrease in platelet count by at least 30% of baseline levels.
- Drug interactions. Because oral anticoagulants interact with many other medications and herbal and nutritional supplements, close monitoring of the patient’s medication schedule is necessary.
Assessment and Diagnostic Findings
Detecting early signs of venous disorders of the lower extremities may be possible through:
- Doppler ultrasound. The tip of the Doppler transducer is positioned at a 45- to 60-degree angle over the expected location of the artery and angled slowly to identify arterial blood flow.
- Computed tomography. Computed tomography provides cross-sectional images of soft tissue and visualizes the area of volume changes to an extremity and the compartment where changes take place.
The objectives for treatment of DVT are to prevent thrombus from growing and fragmenting, recurrent thromboemboli, and postthrombotic syndrome
- Endovascular management. Endovascular management is necessary for DVT when anticoagulant or thrombolytic therapy is contraindicated, the danger of pulmonary embolism is extreme, or venous drainage is so severely compromised that permanent damage to the extremity is likely.
- Vena cava filter. A vena cava filter may be placed at the time of thrombectomy; this filter traps late emboli and prevents pulmonary emboli.
Pharmacologic Therapy
Measures for preventing or reducing blood clotting within the vascular system are indicated in patients with deep vein thrombosis.
- Unfractionated heparin. Unfractionated heparin is administered subcutaneously to prevent development of DVT, or by intermittent or continuous IV infusion for 5 days to prevent the extension of a thrombus and the development of new thrombi.
- Low-molecular-weight heparin (LMWHs). Subcutaneous LMWHs that may include medications such as dalteparin and enoxaparin are effective treatments for some cases of DVT; they prevent the extension of a thrombus and development of new thrombi.
- Oral anticoagulants. Warfarin is a vitamin K antagonist that is indicated for extended coagulant therapy.
- Factor Xa inhibitor. Fondaparinux selectively inhibits factor Xa.
- Thrombolytic therapy. Unlike heparins, catheter-directed thrombolytic therapy lyses and dissolves thrombi in at least 50% of patients.
Nursing management for deep vein thrombosis entails the following:
Nursing Assessment
Assessment of a patient with deep vein thrombosis include:
- Presenting signs and symptoms. If a patient presents with signs and symptoms of DVT, carrt out an assessment of general medical history and a physical examination to exclude other causes.
- Well’s diagnostic algorithm. Because of the unreliability of clinical features, Well’s diagnostic algorithm has been validated whereby patients are classified as having a high, intermediate, or low probability of developing DVT.
Nursing Diagnosis
Based on the assessment data, the major nursing diagnoses are:
- Ineffective tissue perfusion related to interruption of venous blood flow.
- Impaired comfort related to vascular inflammation and irritation.
- Risk for impaired physical mobility related to discomfort and safety precautions.
- Deficient knowledge regarding pathophysiology of condition related to lack of information and misinterpretation.
Nursing Care Planning & Goals
The major goals for the patient include:
- Demonstrate increased perfusion as individually appropriate.
- Verbalize understanding of condition, therapy, regimen, side effects of medications, and when to contact the healthcare provider.
- Engage in behaviors or lifestyle changes to increase level of ease.
- Verbalize sense of comfort or contentment.
- Maintain position of function and skin integrity as evidenced by absence of contractures, footdrop, decubitus, and so forth.
- Maintain or increase strength and function of affected and/or compensatory body part.
Nursing Interventions
The major nursing interventions that the nurse should observe are:
- Provide comfort. Elevation of the affected extremity, graduated compression stockings, warm application, and ambulation are adjuncts to the therapy that can remove or reduce discomfort.
- Compression therapy. Graduated compression stockings reduce the caliber of the superficial veins in the leg and increase flow in the deep veins; external compression devices and wraps are short stretch elastic wraps that are applied from the toes to the knees in a 50% spiral overlap; intermittent pneumatic compression devices increase blood velocity beyond that produced by the stockings.
- Positioning and exercise. When patient is on bed rest, the feet and lower legs should be elevated periodically above the level of the heart, and active and passive leg exercises should be performed to increase venous flow.
Evaluation
Expected patient outcomes are:
- Demonstrated increased perfusion as individually appropriate.
- Verbalized understanding of condition, therapy, regimen, side effects of medications, and when to contact the healthcare provider.
- Engaged in behaviors or lifestyle changes to increase level of ease.
- Verbalized sense of comfort or contentment.
- Maintained position of function and skin integrity as evidenced by absence of contractures, footdrop, decubitus, and so forth.
- Maintained or increased strength and function of affected and/or compensatory body part.
Discharge and Home Care Guidelines
The nurse must also promote discharge and home care to the patient.
- Drug education. The nurse should teach about the prescribed anticoagulant, its purpose, and the need to take the correct amount at the specific times prescribed.
- Blood tests. The patient should be aware that periodic blood tests are necessary to determine if a change in medication or dosage is required.
- Avoid alcohol. A person who refuses to discontinue the use of alcohol should not receive anticoagulants because chronic alcohol intake decreases their effectiveness.
- Activity. Explain the importance of elevating the legs and exercising adequately.
Documentation Guidelines
The focus of documentation include:
- Nature, extent, and duration of the problem, effect on indepence and lifestyle.
- Characteristics of discomfort.
- Pulses and BP.
- Factors impacting sense of discomfort.
- Medication use and nonpharmacological measures
Plan of care
- Teaching plan.
- Response to interventions, teaching, and actions performed.
- Attainment or progress towards desired outcomes.
- Modifications to plan of care.
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Deep Vein Thrombosis: Causes, Symptoms And Treatment
Deep Vein Thrombosis Of The Upper Limbs: How To Deal With A Patient With Paget-Schroetter Syndrome
Allergy/Hypersensitivity To Heparin(S)
Venous Thrombosis: From Symptoms To New Drugs
COVID-19, The Mechanism Of Arterial Thrombus Formation Discovered: The Study
The Incidence Of Deep Vein Thrombosis (DVT) In Patients With MIDLINE
Deep Vein Thrombosis Of The Upper Limbs: How To Deal With A Patient With Paget-Schroetter Syndrome
Knowing Thrombosis To Intervene On The Blood Clot
Venous Thrombosis: What It Is, How To Treat It And How To Prevent It
Pulmonary Thromboembolism And Deep Vein Thrombosis: Symptoms And Signs
Summer Heat And Thrombosis: Risks And Prevention
Raising The Bar For Pediatric Trauma Care: Analysis And Solutions In The US
Deep Vein Thrombosis: Causes, Symptoms And Treatment



