Inguinal hernia: symptoms and treatment
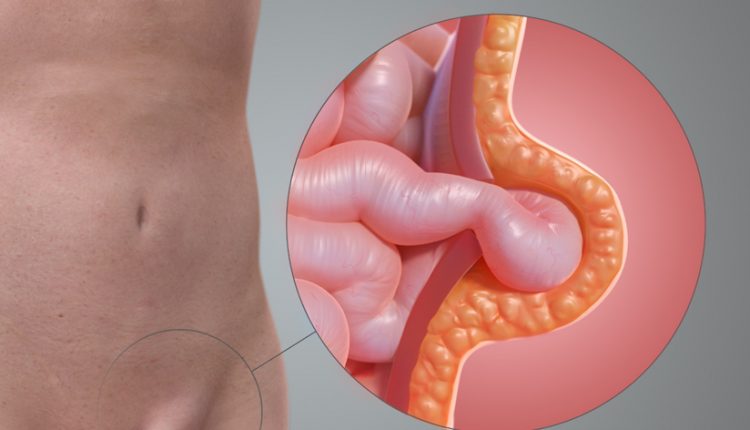
An inguinal hernia is the leakage of abdominal viscera through an area of wall weakness, due to the presence of the inguinal canal
This canal allows the passage of blood vessels to the testicles and the spermatic duct and is located just above the inguinal fold.
The viscera surrounded by a peritoneal sac penetrate from inside the abdominal cavity, through the internal inguinal ring, along this canal and exit through an opening, the external inguinal ring, located near the pubis.
Types of inguinal hernias
Inguinal hernias are most frequently found on the right side for unknown reasons.
They are classified into external, direct and internal oblique hernias.
This subdivision has no significance with regard to either the picture of symptoms or the choice of treatment.
Who is more likely to suffer from inguinal hernia?
Inguinal hernias are ten times more common in men than in women and are increasingly found with advancing age.
This is reflected in the figure, taken from a national register, which reports a frequency of inguinal hernia surgery of 0.25 per cent at the age of 18, rising to 4 per cent from 75 to 80.¹
In addition to male gender and age, a risk factor noted is familiarity: those who have ancestors and direct relatives with hernia have an 8-fold increased risk of having an inguinal hernia compared to those who do not.²
Patients who are overweight or obese are more likely to develop an inguinal hernia than those who are underweight.³
Other favourable conditions are the presence of chronic obstructive bronchitis and smoking, probably due to the effect of repeated coughing resulting in increased intra-abdominal pressure, the presence of aortic aneurysms and diseases of the connective tissue.
The opinion that lifting weights may promote the formation of inguinal hernia is not supported by scientific data; moreover, there is no evidence of an increased incidence of inguinal hernia in weightlifters.4
What causes inguinal hernia formation?
The causal factor most likely linked to the occurrence of inguinal hernia is an alteration in the composition of collagen, the component of connective tissue primarily responsible for its strength and firmness.
Studies to this effect have been undertaken, but at present, there are no mechanisms that are definitely believed to be responsible for these alterations in collagen, and above all, there are no glimmers of a possible effective therapeutic strategy.
What are the characteristic symptoms of an inguinal hernia?
In about a third of patients, there are no symptoms but only a swelling that emerges when standing and after exertion and disappears when lying down.
The most frequent symptom is pain, sometimes continuous and dull and sometimes sharp, especially after coughing, straining and sexual acts.
The pain is often worse at the end of the day and is relieved by assuming the supine position or by retracting the hernia in the abdomen with manual manoeuvres.
If the pain occurs acutely, is not relieved by lying on one’s back, and is associated with the presence of a painful, tense inguinal swelling that cannot be reduced even with manual manoeuvres, the suspicion of hernia stricture must be raised, requiring urgent medical evaluation and possible surgical intervention to avoid serious complications such as intestinal perforation.
In the case of reducible inguinal swelling, the diagnosis is obvious and does not require further investigation with ultrasound or tomography.
These examinations may only be necessary when the typical features of an inguinal hernia, outlined above, are not present to rule out occult hernias or other pathologies.
How is an inguinal hernia treated?
Inguinal hernias that cause symptoms that interfere with the patient’s quality of life must be operated on.
In the case of a hernia without associated symptoms, one may also choose not to operate, especially in patients with other pathologies that make surgery risky.
In women, as it is often difficult to differentiate an inguinal hernia from a crural hernia, it is preferred to indicate surgery even in the absence of symptoms.
This strategy is justified by the fact that crural hernias have a high risk of becoming strangulated and requiring urgent surgery.5
Inguinal hernia repair surgery involves the application of a synthetic mesh to close the wall defect.
The operation can be performed with an inguinal incision under local anaesthesia and without the need for hospitalisation, or laparoscopically under general anaesthesia with three small incisions.
Laparoscopic surgery has the following advantages
- easier intervention in the presence of a recurring hernia
- possibility of performing bilateral hernia repair using only three small skin incisions as for unilateral hernias;
- faster postoperative recovery.
In terms of effectiveness, both traditional and laparoscopic repair are superimposable.
In patients with comorbidities, the technique under local anaesthesia is preferred, because it is less invasive.
The laparoscopic procedure is more technically complex and requires surgeons with sufficient experience to guarantee optimal results.
Chronic postoperative pain at the surgical site is very frequent, affecting about 1 in 10 patients, and in half of these cases it is also disabling.
The laparoscopic technique does not appear to provide any advantages over the traditional technique in this area.
Inguinal Hernia, Prevention Tips
The use of hernia-containing devices such as belts and special pants is widespread, but there are no studies documenting their effectiveness in reducing symptoms and preventing complications.7
Bibliography
Burcharth J, Pedersen M, Bisgaard T, Pedersen C, Rosenberg J. Nationwide prevalence of groin hernia repair. PLoS One 2013; 8: e54367.
Burcharth J, Pommergaard HC, Rosenberg J. The inheritance of groin hernia: a systematic review. Hernia 2013;17:183-9.
de Goede B, Timmermans L, van Kempen BJ, van Rooij FJ, Kazemier G, Lange JF, Hofman A, Jeekel J. Risk factors for inguinal hernia in middle-aged and elderly men: results from the Rotterdam Study. Surgery. 2015;157:540-6.
Ruhl CE, Everhart JE. Risk factors for inguinal hernia among adults in the US population. Am J Epidemiol 2007; 165:1154-61.
Fitzgibbons RJ Jr, Forse RA Clinical practice. Groin hernias in adults. N Engl J Med. 2015;372:756-63.
Simons MP, Aufenacker T, Bay-Nielsen M, Bouillot JL, Campanelli G, Conze J, de Lange D, Fortelny R, Heikkinen T, Kingsnorth A, Kukleta J, Morales-Conde S, Nordin P, Schumpelick V, Smedberg S, Smietanski M, Weber G, Miserez M. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2009;13:343-403.
Whitaker J, Akritidis G, Baker D. Who’s trusting in a truss?. Hernia. 2014;18:147-8.
Read Also:
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
What It Is And How To Recognise Abdominal Diastasis
Chronic Pain And Psychotherapy: The ACT Model Is Most Effective
Hiatal Hernia: What It Is And How To Diagnose It
Percutaneous Discectomy For Herniated Discs
What Is That Swelling? Everything You Need To Know About Inguinal Hernia
Symptoms And Causes Of Umbilical Hernia Pain



