Gastro-cardiac syndrome (or Roemheld syndrome): symptoms, diagnosis and treatment
Gastro-cardiac syndrome, also known as ‘Roemheld-Techlenburg-Ceconi syndrome’ or ‘gastric fundus hyperdistension syndrome’, was first reported by Ludwing Roemheld (1871-1938) in the late 1900s. It is little described in the literature, but is well known to cardiologists and gastroenterologists
What is gastro-cardiac syndrome?
Gastro-cardiac syndrome is characterised by a complex of functional cardiac disorders triggered by gastric distension.
The cardio-respiratory symptoms are often of such intensity as to alarm the patient who, on suspicion of a real cardiac pathology, immediately turns to the cardiologist or emergency room.
However, once a cardiological liability has been ruled out, the patient is sent to the gastroenterologist for diagnosis and treatment of the underlying digestive pathology.
What are the symptoms?
The symptoms of Roemheld Syndrome, which generally appear after meals, are diverse and variously associated with each other:
- chest pain
- difficulty breathing
- severe discomfort at the ‘mouth’ of the stomach
- gastric distension (often evident in the epigastrium and/or left hypochondrium),
- nausea,
- asthenia,
- feeling of fainting,
- difficulty eructating,
- sweating,
- anxiety,
- more or less intense palpitations
- difficulty sleeping (especially if you go to sleep a few hours after a meal or lie on your left side).
It is important to emphasise that the symptomatology is not determined by any cardiological pathology, nor can the symptoms impair cardiac function as the syndrome persists.
What are the causes of gastro-cardiac syndrome?
Although the mechanisms by which gastro-cardiac reflexes are triggered are not well understood, it seems that the trigger for gastro-cardiac syndrome is an excess of air in the stomach and in particular in the gastric fundus.
The severely distended stomach can cause the diaphragm, that flat, dome-shaped muscle that separates the chest from the abdomen and the thoracic organs from the abdominal organs, to rise.
The heart, which rests on the diaphragm and is in close contiguity with the gastric fundus, is in turn pushed upwards.
This displacement of the heart muscle causes the activation of ‘reflex’ responses (i.e. independent and involuntary activities) that can lead to the symptoms described above.
Regardless of the mechanical action on the diaphragm and heart, however, it appears that gastric distension alone can activate reflexes (called ‘gastro-cardiac reflexes’) that can lead to the onset of symptomatology.
To recognise Roemheld syndrome there are no specific tests, but it is a ‘diagnosis of exclusion’
First of all, a specialist cardiological consultation is essential in order to rule out a possible cardiac pathology.
From the gastroenterological point of view, then, any pathologies that may cause or aggravate intestinal meteorism or alter digestive motility must be researched and corrected.
Once organic cardiological and digestive pathologies have been ruled out, the patient should not be considered (as is often the case) a hypochondriac, but a functional syndrome should be suspected and appropriate measures put in place to reduce stomach bloating and promote effective digestive motility, should this be deficient.
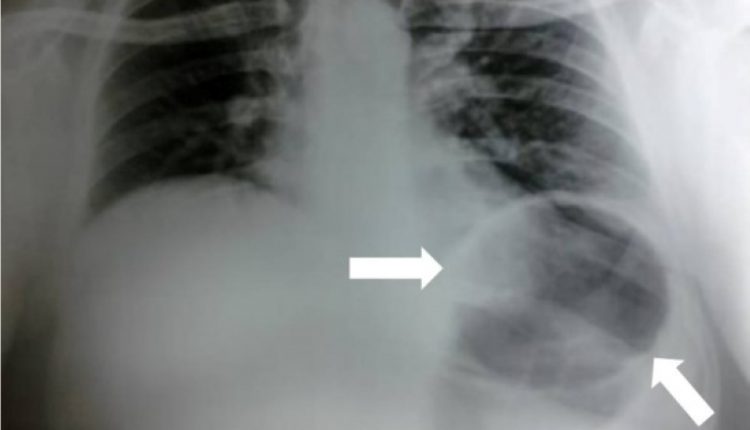
Confirmation of gastric distension (sometimes considerable) can be obtained by a direct X-ray of the abdomen at the time of the crisis.
The prevention of gastro-cardiac syndrome
Since, as already mentioned, the triggering cause seems to be related to gastric distension (the patient often finds immediate relief by belching!) it is necessary to ‘focus’ on the conditions that can lead to ‘stomach bloating’.
It is important, therefore, to eliminate certain ‘bad habits’ about eating behaviour, and then move on to ‘what’ one eats.
Here, in summary, are some general rules to avoid ‘stomach bloating’:
- Maintain a healthy weight by taking regular daily exercise.
- Do not smoke.
- Limit alcohol.
- Eat little, several times a day, to avoid overloading the stomach: concentrating all the food in one meal is the equivalent of concentrating a whole day’s work in a few hours!
- Eat slowly and chew for a long time to avoid swallowing air that distends the stomach.
- One must also remember that the first digestion takes place in the mouth, so eating in a hurry without chewing the food well results in longer gastric work.
- Limit very spicy foods and acidic foods such as tomatoes and citrus fruits.
- Never eat until you feel completely full.
- Try to eat ‘calmly’ and if you are at work, avoid eating quickly and standing up: eat your meal calmly, if possible sitting down, giving yourself at least 20-30 minutes to relax before resuming work.
- Do not wear clothes that are too tight, especially at the table.
- Moderate the use of drinks containing caffeine (such as chocolate, coffee, tea).
- Take a walk after meals and avoid ‘lying down’ immediately.
On the basis of the patient’s medical history, the gastroenterologist will indicate specific corrective measures to the patient and, if necessary, prescribe targeted pharmacological treatment (prokinetics, antimeteorics, etc.).
If this approach proves insufficient or ineffective, the patient’s psychological state must then be assessed and, if necessary, psychotherapeutic support recommended.
What to do during a crisis?
The first rule is not to panic.
The fundamental thing is to know that it is a functional disorder and that nothing can happen.
Being aware of what you have is already half a therapy.
THE WORLD’S RESCUE RADIO? IT’S RADIOEMS: VISIT ITS BOOTH AT EMERGENCY EXPO
Some tricks to control gastro-cardiac syndrome:
Lie down on a bed and breathe deeply and slowly.
Take some anxiolytics if necessary.
Try to eliminate air from the stomach by finding a suitable position (changing the decubitus, etc.) or by taking a warm or slightly fizzy drink.
Light diet in the following hours.
Bibliographic references
- Ursprungsanomalie der rechten Koronararterie und Roemheld-Syndrom – L. Hagemeier – Rechtsmedizin (Springer Medizin Verlag) 2009; 19:30-33.
- Il “peso sullo stomaco”, ossia la cattiva digestione – F. Cosentino, Medicitalia
- Il reflusso gastroesofageo… a tavola! – F. Cosentino, Medicitalia
- La dieta FODMAP per combattere il meteorismo – F. Cosentino, Medicitalia
Read Also
Emergency Live Even More…Live: Download The New Free App Of Your Newspaper For IOS And Android
Supraventricular Tachycardia: Definition, Diagnosis, Treatment, And Prognosis
Ventricular Aneurysm: How To Recognise It?
Atrial Fibrillation: Classification, Symptoms, Causes And Treatment
EMS: Pediatric SVT (Supraventricular Tachycardia) Vs Sinus Tachycardia
Atrioventricular (AV) Block: The Different Types And Patient Management
Pathologies Of The Left Ventricle: Dilated Cardiomyopathy
A Successful CPR Saves On A Patient With Refractory Ventricular Fibrillation
Atrial Fibrillation: Symptoms To Watch Out For
Atrial Fibrillation: Causes, Symptoms And Treatment
Difference Between Spontaneous, Electrical And Pharmacological Cardioversion
‘D’ For Deads, ‘C’ For Cardioversion! – Defibrillation And Fibrillation In Paediatric Patients
Inflammations Of The Heart: What Are The Causes Of Pericarditis?
Do You Have Episodes Of Sudden Tachycardia? You May Suffer From Wolff-Parkinson-White Syndrome (WPW)
Knowing Thrombosis To Intervene On The Blood Clot
Patient Procedures: What Is External Electrical Cardioversion?
Increasing The Workforce Of EMS, Training Laypeople In Using AED
Heart Attack: Characteristics, Causes And Treatment Of Myocardial Infarction
Altered Heart Rate: Palpitations
Heart: What Is A Heart Attack And How Do We Intervene?
Do You Have Heart Palpitations? Here Is What They Are And What They Indicate
Palpitations: What Causes Them And What To Do
Cardiac Arrest: What It Is, What The Symptoms Are And How To Intervene
Electrocardiogram (ECG): What It Is For, When It Is Needed
What Are The Risks Of WPW (Wolff-Parkinson-White) Syndrome
Heart Failure: Symptoms And Possible Treatments
What Is Heart Failure And How Can It Be Recognised?
Inflammations Of The Heart: Myocarditis, Infective Endocarditis And Pericarditis
Quickly Finding – And Treating – The Cause Of A Stroke May Prevent More: New Guidelines
Atrial Fibrillation: Symptoms To Watch Out For
Wolff-Parkinson-White Syndrome: What It Is And How To Treat It
Do You Have Episodes Of Sudden Tachycardia? You May Suffer From Wolff-Parkinson-White Syndrome (WPW)
What Is Takotsubo Cardiomyopathy (Broken Heart Syndrome)?
Heart Disease: What Is Cardiomyopathy?
Inflammations Of The Heart: Myocarditis, Infective Endocarditis And Pericarditis
Heart Murmurs: What It Is And When To Be Concerned
Broken Heart Syndrome Is On The Rise: We Know Takotsubo Cardiomyopathy
Heart Attack, Some Information For Citizens: What Is The Difference With Cardiac Arrest?
Heart Attack, Prediction And Prevention Thanks To Retinal Vessels And Artificial Intelligence
Full Dynamic Electrocardiogram According To Holter: What Is It?
In-Depth Analysis Of The Heart: Cardiac Magnetic Resonance Imaging (CARDIO – MRI)
Palpitations: What They Are, What Are The Symptoms And What Pathologies They Can Indicate
Cardiac Asthma: What It Is And What It Is A Symptom Of
Cardiac Rhythm Restoration Procedures: Electrical Cardioversion
Abnormal Electrical Activity Of The Heart: Ventricular Fibrillation



